Many people over 65 take medications for common issues like allergies, overactive bladder, depression, or insomnia. What they don’t realize is that some of these everyday drugs could be quietly harming their brain. Anticholinergic medications - which block a key brain chemical called acetylcholine - are linked to faster memory loss and a higher chance of developing dementia. This isn’t just a theory. Large, long-term studies show a clear pattern: the more of these drugs you take, and the longer you take them, the greater your risk.
What Are Anticholinergic Medications?
Anticholinergic drugs work by blocking acetylcholine, a neurotransmitter that helps nerves communicate. This is useful for treating conditions like muscle spasms, excessive sweating, or overactive bladder. But in the brain, acetylcholine is also vital for memory, attention, and learning. When these drugs cross the blood-brain barrier, they interfere with those functions. Common examples include:- Diphenhydramine (Benadryl) - used for allergies and sleep
- Oxybutynin (Ditropan) - for overactive bladder
- Amitriptyline (Elavil) - an older antidepressant
- Hyoscyamine - for stomach cramps
- Chlorpheniramine - found in many cold and allergy meds
How Strong Is the Link to Dementia?
It’s not a small risk. A major 2019 study using France’s national health database tracked over 1,000 people for more than a decade. They found that those who took the equivalent of 1,095 daily doses - roughly three years of daily use - had a 49% higher risk of developing dementia compared to people who didn’t take these drugs at all. The risk didn’t jump all at once. It built up slowly:- 1-90 doses: 6% higher risk
- 91-365 doses: 19% higher risk
- 366-1,094 doses: 33% higher risk
- Over 1,095 doses: 49% higher risk
Not All Anticholinergics Are the Same
Some medications carry much higher risk than others. The type of drug matters more than you might think. According to a 2019 JAMA Internal Medicine study:- Antidepressants (especially tricyclics like amitriptyline): 29% higher dementia risk
- Antipsychotics: 20% higher risk
- Bladder drugs (oxybutynin, solifenacin): 13-20% higher risk
- Anti-Parkinson drugs: 10% higher risk

Who’s Most at Risk?
The risk isn’t the same for everyone. Older adults - especially those over 70 - are most vulnerable. But other factors make it worse:- People taking multiple anticholinergic drugs at once
- Those with genetic risk for Alzheimer’s, like the APOE-ε4 gene variant
- Individuals already showing early memory problems
- People with other health issues like diabetes, high blood pressure, or depression
What Do Doctors Know?
Surprisingly, many don’t check for anticholinergic burden. A 2021 survey by the American Geriatrics Society found that only 37% of primary care doctors routinely screen for these drugs in patients over 65 - even though nearly 90% say they understand the risk. Why the gap? Time, lack of tools, and unclear guidelines. But things are changing. The American Geriatrics Society’s Beers Criteria® (updated in 2019) now explicitly says: “Avoid strong anticholinergics in older adults.” Electronic health record systems like Epic now include built-in anticholinergic burden calculators that flag risky combinations. Still, many patient medication leaflets don’t mention cognitive risks - even though EU regulations require it since 2017. Only 42% of them do.What Can You Do?
You don’t have to stop all your meds overnight. But you can take smart steps:- Review all your meds - including OTC pills, supplements, and sleep aids. Write them all down.
- Ask your doctor: “Is this drug anticholinergic? Is there a safer alternative?”
- Look for alternatives:
- For insomnia: Try cognitive behavioral therapy (CBT-I) instead of diphenhydramine
- For overactive bladder: Switch from oxybutynin to mirabegron (Myrbetriq) - it has zero anticholinergic effect
- For depression: Consider SSRIs like sertraline instead of amitriptyline
- For allergies: Use loratadine or cetirizine instead of diphenhydramine
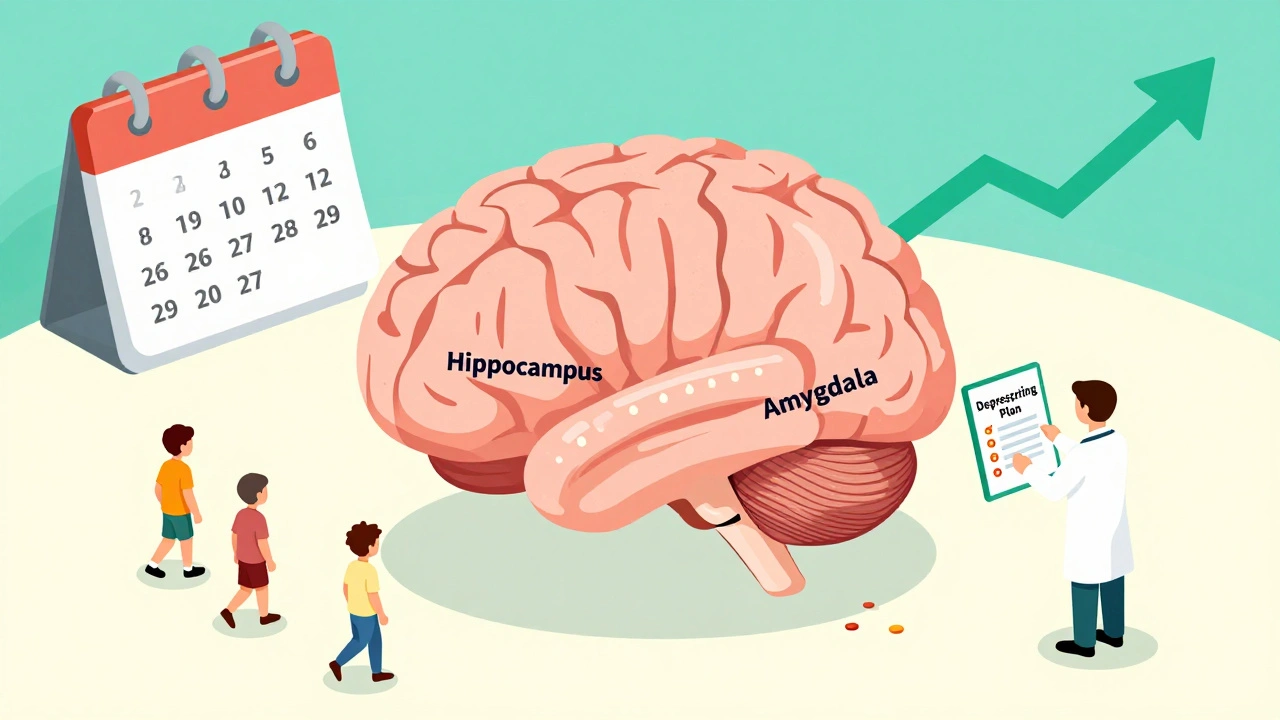
Deprescribing Is a Process
Stopping these drugs suddenly can cause withdrawal symptoms - increased heart rate, sweating, nausea, or even rebound bladder problems. That’s why tapering is essential. The Canadian Deprescribing Guidelines recommend reducing doses slowly over 4 to 8 weeks. Your doctor can help you create a safe plan. Don’t quit cold turkey.What’s Being Done About It?
The Alzheimer’s Association estimates that reducing anticholinergic use could prevent 10-15% of dementia cases each year - roughly 570,000 people globally. The American Geriatrics Society launched the Anticholinergic Risk Reduction Initiative in 2022. Their goal: cut inappropriate prescribing by 50% by 2027. Meanwhile, drug companies are developing new medications that treat the same conditions without affecting the brain. Seven new bladder treatments and three new antidepressants are in late-stage trials - all designed to avoid crossing into the brain.Bottom Line
Anticholinergic medications aren’t evil. They help people with real, sometimes urgent, health problems. But they’re not harmless, especially over time. For older adults, the cost to memory and brain health can be high. If you or a loved one is taking any of these drugs, don’t panic. But do ask questions. Ask for alternatives. Ask for a review. Small changes - like switching from Benadryl to a non-sedating antihistamine - can make a real difference. The brain doesn’t recover quickly. But it can be protected - if we act before it’s too late.Can anticholinergic drugs cause dementia, or just temporary confusion?
They can cause both. Short-term use may lead to temporary brain fog, dry mouth, or dizziness. But long-term use - especially over three years - is linked to lasting brain changes. Studies show increased brain shrinkage, reduced glucose use in memory areas, and higher rates of dementia diagnosis. The damage isn’t always reversible, even after stopping the drug.
Are all over-the-counter sleep aids anticholinergic?
No, but many are. Diphenhydramine (found in Benadryl, Tylenol PM, ZzzQuil) and doxylamine (Unisom) are strong anticholinergics. Look for products labeled “non-drowsy” - those usually contain melatonin or valerian root instead. Always check the active ingredients. If it says “antihistamine,” it’s likely anticholinergic.
Is there a test to measure anticholinergic burden?
Yes. Doctors can use the Anticholinergic Cognitive Burden (ACB) scale or the Anticholinergic Risk Scale (ARS). These tools assign points based on drug type and dose. A score of 3 or higher is considered high risk. Many electronic health records now calculate this automatically when prescribing.
Can stopping anticholinergic drugs improve memory?
Yes, in many cases. Studies show that people who stop these drugs often see improvements in attention, processing speed, and memory within weeks to months. While full recovery isn’t guaranteed - especially after long-term use - cognitive decline often slows or stabilizes. The earlier you stop, the better the chance of improvement.
What are the safest alternatives to oxybutynin for overactive bladder?
Mirabegron (Myrbetriq) is the top alternative. It works differently - by relaxing the bladder muscle without blocking acetylcholine - and has an ACB score of 0. Other options include behavioral therapies like timed voiding, pelvic floor exercises, and bladder training. In some cases, Botox injections into the bladder are used. Always discuss these with your doctor.
James Kerr
December 2, 2025 AT 02:28Wow, this is eye-opening. I had no idea my nightly Benadryl for sleep was basically a slow-motion brain drain. 😅 Switched to melatonin last month and honestly? Better sleep, clearer head. Who knew?
shalini vaishnav
December 3, 2025 AT 21:24This is typical Western medical ignorance. In India, we’ve been using ayurvedic remedies for centuries without destroying cognition. Why are you so quick to abandon traditional wisdom for pharmaceutical snake oil?
vinoth kumar
December 4, 2025 AT 02:04Really appreciate this breakdown! I’ve been helping my dad sort through his meds after he started forgetting names. We found three anticholinergics he’d been on for years - including amitriptyline for nerve pain. He’s been on mirabegron for bladder issues for two months now and says he feels like he’s 10 years younger. Seriously, talk to your doctor!
bobby chandra
December 4, 2025 AT 11:42Let’s be crystal clear: this isn’t just a ‘risk’ - it’s a silent epidemic disguised as a pill bottle. We’re handing out brain grenades labeled ‘for sleep’ and ‘for allergies’ like candy. And then we wonder why dementia rates are skyrocketing. It’s not aging - it’s pharmacology. Time to stop blaming neurons and start blaming prescriptions.
Archie singh
December 5, 2025 AT 21:20Of course the pharmaceutical industry doesn’t want you to know this. They profit from chronic conditions. They don’t care if you forget your grandkids’ names as long as you keep refilling. Wake up. The system is rigged.
Gene Linetsky
December 6, 2025 AT 16:58They’re hiding this from us on purpose. Did you know the FDA approved diphenhydramine as OTC in 1982 without a single cognitive study? Coincidence? Or corporate cover-up? I’ve got sources. You should dig deeper.
Kidar Saleh
December 8, 2025 AT 02:57I’ve seen this in my practice in London. An elderly patient came in with memory complaints - turned out she’d been taking chlorpheniramine for hay fever for 12 years. We switched her to loratadine. Within six weeks, she was remembering her own birthday again. It’s not magic. It’s just science.
Chloe Madison
December 9, 2025 AT 08:09This information is not merely valuable - it is potentially life-altering. I urge every individual over the age of 60, and their caregivers, to conduct a comprehensive medication review with a geriatric pharmacist. The cognitive preservation potential is immense, and the cost of inaction is irreparable.
Vincent Soldja
December 11, 2025 AT 01:48Interesting. But where’s the data on confounding variables? Many of these patients have depression, diabetes, poor sleep - all of which independently increase dementia risk. Correlation isn’t causation.
Rashmin Patel
December 11, 2025 AT 10:17As someone who’s watched my grandmother decline over 8 years, I can tell you this isn’t just about pills - it’s about how we treat our elders. We give them meds to fix every symptom without asking if the fix is worse than the problem. I switched her from oxybutynin to mirabegron and started her on pelvic floor exercises. She’s laughing again. That’s worth more than any pill. 🙏❤️
Cindy Lopez
December 13, 2025 AT 07:51They didn’t mention the dose-response curve for anticholinergics in combination. That’s where the real danger lies. Taking two low-risk drugs can equal one high-risk one. That’s the hidden trap.
Ignacio Pacheco
December 14, 2025 AT 09:06So… we’re supposed to believe that a drug that makes you sleepy is also quietly shrinking your hippocampus? And no one told us this because…? Because we’re too dumb to read the tiny print on the bottle?
Rashi Taliyan
December 14, 2025 AT 19:35I’m so grateful this was posted. My mother was on amitriptyline for 10 years. We didn’t realize the fog was the drug - we thought it was just aging. When she stopped, she remembered how to play the piano again. That’s not recovery. That’s resurrection.
Kara Bysterbusch
December 15, 2025 AT 00:49This is one of the most critical public health messages of our time - and yet, it’s buried under a mountain of marketing, inertia, and medical complacency. The fact that 63% of doctors don’t screen for anticholinergic burden is not an oversight - it’s a systemic failure. We must demand better. Our brains are not collateral damage.