Diabetes & Sexual Health Symptom Checker
This tool helps identify common diabetes-related sexual health symptoms and suggests immediate actions based on gender. Remember, this is for informational purposes only and not a substitute for professional medical advice.
Your Results
Common Symptoms & Actions
Erectile Dysfunction
Reduced blood flow and nerve damage from diabetes can lead to difficulty achieving or maintaining an erection.
Vaginal Dryness
Decreased blood flow and hormonal changes can cause discomfort and reduced lubrication during intercourse.
Low Libido
Fluctuating blood sugar, hormonal imbalances, and emotional stress can significantly reduce sexual desire.
Delayed Arousal
Nerve damage and reduced blood flow make it harder to get aroused quickly.
TL;DR
- High blood sugar can damage nerves and blood vessels, leading to erectile dysfunction in men and vaginal dryness in women.
- Hormonal shifts and certain diabetes meds also play a role.
- Good glucose control, regular exercise, and open talks with doctors can improve intimacy.
- Therapies such as PDE5 inhibitors, lubricants, and counseling are effective for many.
- Addressing mental health is a key part of any treatment plan.
When you hear the phrase diabetes and sexual health, the first image that often pops up is a medical chart. But behind those numbers are real people who want to feel close to their partners. Diabetes isn’t just about blood sugar; it silently reshapes the way our bodies respond to intimacy. This guide walks through the science, the symptoms you might notice, and practical steps you can take right now.
What Diabetes Does to the Body (in a Nutshell)
Understanding the impact starts with a quick look at the disease itself. Diabetes is a chronic condition where the body either doesn’t produce enough insulin or can’t use it efficiently, causing elevated blood glucose levels. Over time, that extra glucose attacks tiny blood vessels and nerves throughout the body.
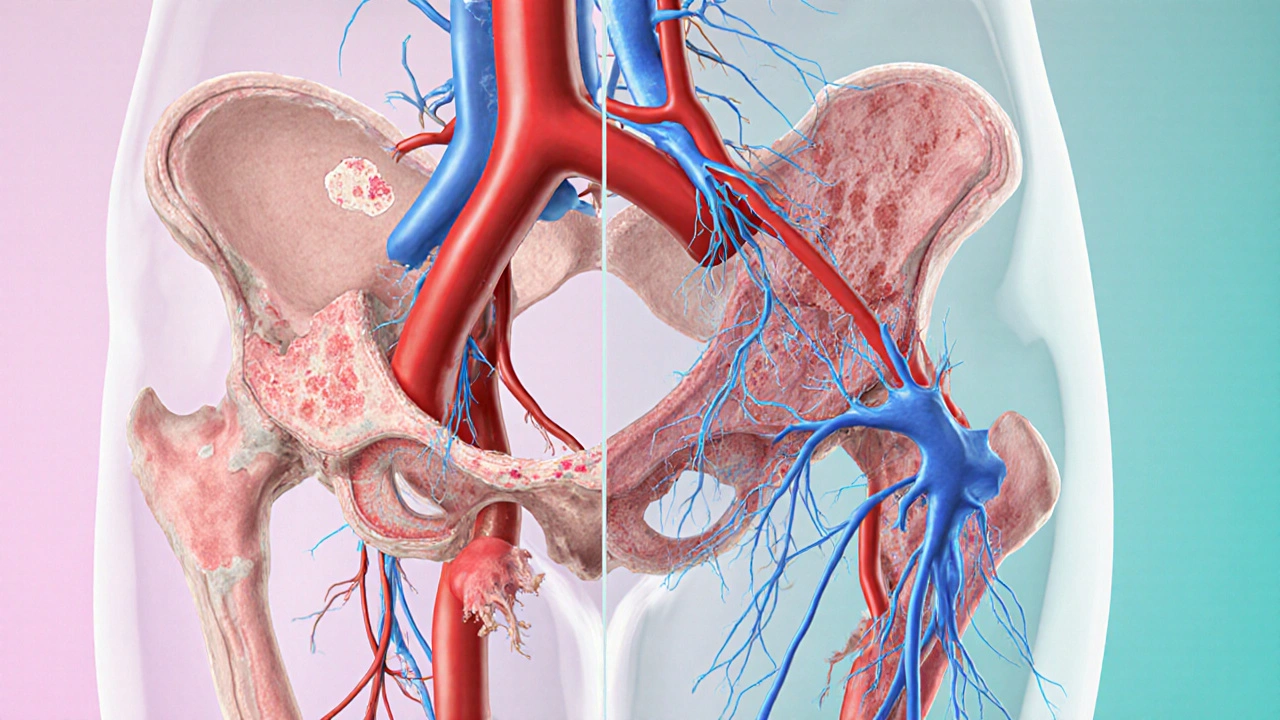
Two physiological culprits matter most for sexual function:
- Vascular disease: Hardened arteries reduce blood flow to the penis and clitoral tissues, making arousal harder.
- Neuropathy: Nerve damage dulls sensation, so the brain receives weaker signals about touch.
Both problems are dose‑dependent-better glucose control usually means less damage.
How Men Experience Sexual Changes
In men, the most common issue is erectile dysfunction (ED), defined as the persistent inability to achieve or maintain an erection sufficient for intercourse. Studies from the American Diabetes Association show that men with type2 diabetes are up to three times more likely to develop ED than non‑diabetic peers.
Key drivers:
- Reduced blood flow: High glucose ages the lining of blood vessels, limiting the rush of blood needed for an erection.
- Impaired nerve signaling: Peripheral neuropathy blunts the sensory feedback that tells the brain it’s time to respond.
- Hormonal imbalance: Diabetes can lower testosterone, further weakening libido.
- Medication side effects: Some antihypertensives and antidepressants, commonly prescribed to diabetics, can worsen ED.
Typical warning signs include a gradual decline in erection quality, longer recovery time after ejaculation, or a complete loss of spontaneous erections (the “morning wood”).
How Women Experience Sexual Changes
Women often notice vaginal dryness, reduced lubrication, and lowered sexual desire. Unlike men, the problem isn’t always as visible, so many women blame stress or relationship issues instead of an underlying health condition.
What’s happening under the hood?
- Reduced blood flow: The same vascular stiffening that affects men also limits the engorgement of clitoral tissue, decreasing arousal.
- Neuropathy: Nerve damage dulls sensation, making touch feel less pleasurable.
- Hormonal shifts: Diabetes can disrupt estrogen levels, which are crucial for maintaining vaginal mucosa.
- Medication: Certain diabetes drugs, especially some thiazolidinediones, have been linked to lower libido.
Early clues include a need for more foreplay, a quick onset of discomfort during intercourse, or a general lack of interest in sexual activity.
Beyond the Physical: Mental and Emotional Layers
Living with a chronic disease brings anxiety, depression, and a sense of embarrassment-all of which can create a feedback loop that worsens sexual problems. A 2023 survey of 2,400 diabetics found that 45% reported feeling “less attractive” after diagnosis, and that sentiment correlated strongly with lower sexual activity.
Addressing mental health isn’t a nice‑to‑have; it’s a must‑have. Counseling, support groups, or even a simple conversation with a trusted friend can break the negative spiral.
Practical Ways to Protect and Restore Intimacy
Good news: many interventions work, often together. Below is a checklist you can start using today.
- Optimize blood sugar: Aim for an A1C below 7% (or the target your doctor sets). Consistent control slows nerve and vessel damage.
- Exercise regularly: Moderate aerobic activity 150 minutes per week improves circulation and boosts testosterone.
- Balanced diet: Focus on low‑glycemic carbs, lean protein, and healthy fats. Foods rich in omega‑3s (salmon, flaxseed) protect blood vessels.
- Quit smoking: Nicotine compounds vascular disease; quitting can improve erectile function within weeks.
- Review medications: Talk to your prescriber about potential sexual side effects. Sometimes a dose tweak or a switch solves the issue.
- Targeted sexual aids:
- Men: Phosphodiesterase‑5 inhibitors (Viagra, Cialis) are first‑line for diabetic ED when safe.
- Women: Water‑based lubricants, vaginal moisturizers, or prescription estrogen creams help with dryness.
- Pelvic floor therapy: Physical therapists can teach exercises that improve blood flow and muscular control for both sexes.
- Psychological support: Cognitive‑behavioral therapy (CBT) and couples counseling address anxiety, body image, and communication.
Below is a quick comparison of the most common symptoms and suggested first‑step actions for men and women.
| Gender | Typical Symptom | Immediate Action |
|---|---|---|
| Men | Erectile dysfunction | Check A1C, discuss PDE5 inhibitors with doctor |
| Women | Vaginal dryness & reduced libido | Use lubricants, evaluate hormonal levels, schedule a pelvic exam |
Talking to Your Healthcare Team
Bringing up sexual health can feel awkward, but doctors expect these conversations. Here’s a quick script you can adapt:
"I've noticed changes in my sexual response lately-like X for men or Y for women. My blood sugar has been Z. Could these be linked, and what options do I have?"
Make sure you have your recent A1C numbers handy, list any new meds, and be ready to discuss lifestyle habits. The more specific you are, the easier it is for the clinician to pinpoint the cause.
When to Seek Specialized Care
If basic adjustments don’t help within three months, consider seeing a specialist:
- Urologist or endocrinologist for persistent ED or hormonal testing.
- Gynecologist or pelvic floor therapist for chronic vaginal dryness or pain.
- Sex therapist when anxiety or relationship strain dominates the picture.
Specialists can run focused tests-like penile Doppler ultrasound or vaginal pH measurement-and prescribe targeted treatments.
Future Outlook: Emerging Therapies
Research is moving fast. Some promising avenues include:
- Low‑intensity shockwave therapy for diabetic ED, showing improved blood flow in early trials.
- Insulin‑like growth factor (IGF‑1) creams that might protect vaginal tissue, still in phase‑2 studies.
- Continuous glucose monitoring (CGM) integrated with mobile apps that give real‑time alerts for glucose spikes during intimacy, helping couples plan.
While these aren’t standard yet, keeping an eye on the latest guidelines can give you a head‑start when they become widely available.
Quick Reference Checklist
- Monitor A1C regularly.
- Prioritize cardio exercise.
- Quit smoking and limit alcohol.
- Discuss medication side effects with your doctor.
- Use appropriate lubricants or prescription aids.
- Seek counseling if anxiety interferes with intimacy.
Frequently Asked Questions
Can diabetes cause loss of libido?
Yes. Fluctuating blood sugar, hormonal changes, and the emotional stress of managing a chronic disease can all lower sexual desire in both men and women.
Is erectile dysfunction always permanent for diabetics?
No. Many men see improvement after tightening glucose control, losing weight, or using PDE5 inhibitors. Early intervention is key.
What over‑the‑counter products help women with vaginal dryness?
Water‑based lubricants (e.g., Astroglide) and silicone‑based options (e.g., Sliquid) are safe choices. For persistent dryness, a prescription estrogen cream may be recommended.
Does tight glucose control increase the risk of hypoglycemia during sex?
If you’re on insulin or sulfonylureas, an active session can lower blood sugar. Keep a quick‑acting carbohydrate nearby and monitor levels before and after intimacy.
Should I tell my partner about my sexual side effects?
Open communication builds trust and lets both partners explore solutions together-whether it’s trying new positions, using aids, or scheduling doctor visits.
Jonathan Mbulakey
October 3, 2025 AT 18:55Diabetes can quietly affect intimacy, so staying aware is essential.
Warren Neufeld
October 4, 2025 AT 11:35When blood sugar spikes repeatedly, the tiny vessels that supply the genitals become less elastic, leading to reduced blood flow. Nerve damage further dulls sensation, which makes arousal harder to achieve. Maintaining a target A1C can slow these processes, but lifestyle tweaks matter too. Regular aerobic exercise, a balanced diet, and quitting smoking are foundational steps.
Abby VanSickle
October 5, 2025 AT 04:15Understanding the link between diabetes and sexual health begins with recognizing that chronic hyperglycemia damages both vascular and neural pathways. Elevated glucose levels cause endothelial dysfunction, which narrows arteries and hampers the rapid blood flow needed for erection in men or clitoral engorgement in women. Simultaneously, peripheral neuropathy reduces the transmission of touch signals, making stimulation feel muted. Hormonal imbalances, such as lowered testosterone in men and altered estrogen in women, further diminish libido. Certain antidiabetic medications can also have side effects that impact desire or performance, so a medication review with a healthcare provider is prudent. Lifestyle modifications remain the cornerstone: achieving an A1C below the target set by your doctor, engaging in at least 150 minutes of moderate aerobic activity per week, and adhering to a low‑glycemic diet rich in omega‑3 fatty acids. Smoking cessation is critical because nicotine accelerates arterial stiffness, and even occasional alcohol can cause temporary glucose fluctuations that affect responsiveness. Psychological factors should not be overlooked; anxiety and depression are common among people managing a chronic disease and can create a feedback loop that worsens sexual dysfunction. Open communication with a partner fosters trust and allows both parties to explore solutions, such as trying different positions, using water‑based lubricants for women, or discussing PDE5 inhibitors with a physician for men. Pelvic floor physical therapy has emerging evidence supporting improved blood flow and muscular control for both sexes. If basic interventions do not yield improvement within a few months, seeking specialized care-urologists, gynecologists, or sex therapists-can provide targeted diagnostics like penile Doppler studies or hormonal panels. Finally, staying informed about emerging therapies, such as low‑intensity shockwave treatment for erectile dysfunction or topical IGF‑1 creams for vaginal health, ensures you can discuss cutting‑edge options when they become clinically available.
Carys Jones
October 5, 2025 AT 20:55The sheer drama of a condition that silently robs you of intimacy is heartbreaking. One moment you’re confident, the next you’re self‑conscious about every whisper of desire. It’s not just a physical hurdle; it’s an emotional avalanche that can drown any hopeful spark. Ignoring the problem only lets it fester, turning a manageable issue into a permanent scar. The truth is, confronting it head‑on with medical help is the only way to reclaim that lost joy.
Roxanne Porter
October 6, 2025 AT 13:35While the intensity of the experience is undeniable, practical steps can temper the fallout. Prioritizing glucose control and discussing medication side‑effects with a prescriber often yields measurable gains. Moreover, involving a partner in the conversation can transform isolation into shared problem‑solving.
Keisha Moss Buynitzky
October 7, 2025 AT 06:15From a clinical perspective, the interplay between metabolic control and sexual function is well documented. Elevated hemoglobin A1c correlates with both the prevalence and severity of erectile dysfunction and vaginal dryness. Consequently, routine monitoring and timely adjustments to therapy are indispensable. In addition to pharmacologic options, non‑pharmacologic measures such as structured pelvic floor exercises have demonstrated efficacy across genders. Patients should also be encouraged to maintain open dialogues with their partners, as relational dynamics significantly influence outcomes. Ultimately, a multidisciplinary approach-endocrinology, urology or gynecology, and mental health support-offers the best prospect for restoring intimacy.
Shivam yadav
October 7, 2025 AT 22:55I agree, integrating lifestyle changes with medical advice creates a balanced path forward.
pallabi banerjee
October 8, 2025 AT 15:35In many cultures, discussing sexual health remains taboo, which makes education even more vital. Simple, clear explanations about how blood sugar affects nerves and blood flow can empower patients to seek help sooner. Providing culturally sensitive resources helps bridge that gap.
Alex EL Shaar
October 9, 2025 AT 08:15Yo, man, this shit ain’t just about "eat less sugar" – it’s a full‑blown system breakdown. Your arteries get all clogged, nerves go slacker, and suddenly you’re left feeling like a rusty robot. Got meds? Some of ’em downright sabotage your mojo. Even the best‑selling Viagra can be a joke if you’re running on a roller‑coaster glucose train. Bottom line: you gotta get that CGM buzzing, hit the gym, and maybe talk to a doc who actually knows their sh*t.
Anna Frerker
October 10, 2025 AT 00:55Diabetes doesn’t have to erase intimacy.
Kim Nguyệt Lệ
October 10, 2025 AT 17:35Indeed, with proactive management and open communication, couples can preserve a fulfilling sexual relationship despite the challenges posed by diabetes.