Opioid Dosing Calculator for Kidney Patients
Select Your Opioid
Recommended Dose
Why Opioids Are Risky in Kidney Failure
When your kidneys aren’t working well, many drugs don’t clear the way they should. Opioids are no exception. In people with chronic kidney disease (CKD) or end-stage renal disease (ESRD), the body can’t remove opioid metabolites effectively. These leftover compounds build up and can cause serious problems - confusion, muscle twitching, seizures, even breathing that slows to dangerous levels. It’s not just about pain relief anymore. It’s about avoiding harm.
Studies show that between 42% and 85% of kidney patients suffer from chronic pain. Yet, nearly two-thirds of them get too little treatment. Why? Doctors are scared. They know morphine or codeine can turn toxic in failing kidneys. But they also know untreated pain lowers quality of life, worsens sleep, and makes recovery harder. So what’s the answer?
Stop Using These Opioids - They’re Dangerous
Some opioids are simply off-limits in kidney failure. The guidelines are clear: avoid morphine, codeine, meperidine, and propoxyphene at all stages of kidney disease.
- Morphine turns into morphine-3-glucuronide, a metabolite that causes seizures and delirium. Even small doses can become dangerous when GFR drops below 50 mL/min.
- Codeine is metabolized into morphine - so it’s just as risky. Plus, some people are poor metabolizers and get no pain relief, while others turn it into too much morphine too fast.
- Meperidine (pethidine) is the worst offender. Its metabolite, normeperidine, builds up quickly and can trigger seizures even at low doses. It’s banned in CKD patients worldwide.
These aren’t just "use with caution" drugs. They’re red flags. If a patient has a GFR under 30, these should never be prescribed. Yet, a 2019 FDA review found that 68% of opioid labels still don’t mention kidney risks. That means many prescriptions are being written without full awareness.
The Safest Opioids for Kidney Patients
Not all opioids are created equal. Two stand out as the safest choices for patients with advanced kidney disease: fentanyl and buprenorphine.
Fentanyl is mostly broken down by the liver - only 7% leaves the body through the kidneys. That means even in ESRD, it doesn’t accumulate dangerously. Transdermal patches are ideal because they give steady, slow release without spikes in blood levels. But here’s the catch: never start a fentanyl patch in someone who’s never taken opioids before. The risk of overdose is real. Also, avoid fentanyl during hemodialysis - clearance is unpredictable.
Buprenorphine is even better for dialysis patients. About 30% is cleared by the kidneys, but because it’s so strongly bound to proteins and broken down heavily in the liver, it doesn’t build up to toxic levels. No dose adjustment is needed, even on dialysis. It’s also less likely to cause respiratory depression than other opioids. The only downside? It can slightly prolong the QT interval on an ECG, so monitoring is wise, especially if the patient is on other QT-prolonging drugs.
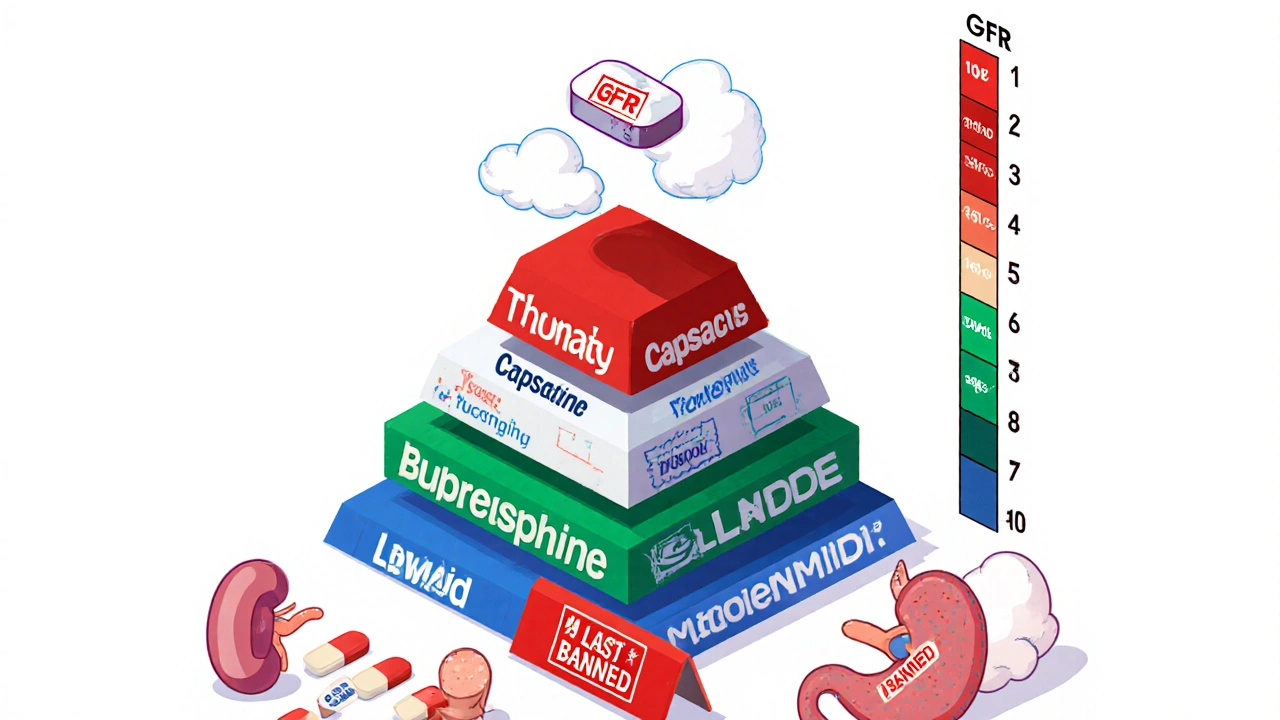
Dosing Adjustments Based on Kidney Function
Even safe opioids need careful dosing. It’s not one-size-fits-all. Your kidney function - measured by GFR or CrCl - determines how much you start with.
| GFR / CrCl | Morphine | Methadone | Fentanyl | Buprenorphine |
|---|---|---|---|---|
| >50 mL/min | 100% usual dose | 100% usual dose | 75-100% usual dose | No adjustment needed |
| 10-50 mL/min | 50-75% usual dose | 100% usual dose | 50-75% usual dose | No adjustment needed |
| <10 mL/min | 25% usual dose | 50-75% usual dose | 50% usual dose | No adjustment needed |
Start low. Go slow. Wait at least 24-48 hours between dose increases. Many doctors make the mistake of rushing to higher doses because the pain isn’t gone right away. But in kidney patients, each increase carries more risk. Patience saves lives.
What About Oxycodone, Hydromorphone, and Tapentadol?
These are trickier. They’re not outright banned, but they come with caveats.
- Oxycodone: About 45% of its metabolites are cleared by the kidneys. In patients with CrCl under 30 mL/min, stick to 20 mg per day max. Monitor closely for drowsiness or confusion.
- Hydromorphone: The parent drug is okay, but its metabolite - hydromorphone-3-glucuronide - builds up in non-dialysis patients and increases neurotoxicity risk by 37%. Use only if no other option exists, and prefer dialysis patients over non-dialysis ones.
- Tapentadol: Safe in mild-to-moderate CKD (CrCl ≥30 mL/min). But there’s no data for ESRD. Don’t use it in dialysis patients unless you’re in a research setting.
None of these are first-line. They’re backup options. Fentanyl and buprenorphine are still the gold standard.
Managing Side Effects - Especially Constipation
Constipation affects 40-80% of kidney patients on opioids. It’s not just uncomfortable - it can lead to bowel obstruction, nausea, and reduced appetite. Standard laxatives often don’t work well because of fluid restrictions.
The best solution? Naldemedine. Unlike other peripherally-acting opioid antagonists (PAMORAs), it doesn’t need dose adjustment in CKD or dialysis. One 0.2 mg tablet daily is safe and effective. It blocks opioid effects in the gut without reducing pain relief. Other PAMORAs like methylnaltrexone or naloxegol require dose changes based on kidney function - making them harder to use.
Also avoid stimulant laxatives long-term. They can worsen electrolyte imbalances. Focus on hydration (within fluid limits), fiber, and movement. Naldemedine is the real game-changer here.
What About Non-Opioid Options?
Before reaching for opioids, consider alternatives. Many kidney patients benefit from:
- Acetaminophen: Safe in CKD if under 3,000 mg/day. Avoid in advanced liver disease.
- Gabapentin or pregabalin: Useful for nerve pain, but both need dose reduction. Gabapentin: 200-700 mg once daily if CrCl <30. Pregabalin: half the usual dose, given every other day.
- Topical lidocaine or capsaicin: Great for localized pain like arthritis or neuropathy. No systemic absorption means no kidney burden.
- Physical therapy and cognitive behavioral therapy: Proven to reduce pain perception and opioid needs over time.
A 2022 study in the Clinical Journal of the American Society of Nephrology found that patients using multimodal therapy (opioid + non-opioid + physical therapy) used 50% less opioid over six months than those on opioids alone.
Monitoring and Long-Term Risks
Even with the safest opioids, you need ongoing checks:
- ECG before starting methadone or buprenorphine - watch for QT prolongation.
- Regular mental status checks - confusion or twitching means metabolite buildup.
- Review all meds - many kidney patients take 10+ drugs. Interactions matter.
And here’s something rarely discussed: long-term opioid use (>90 days) in CKD patients is linked to a 28% faster decline in kidney function. Why? Possibly because opioids reduce blood flow to the kidneys or increase inflammation. That’s not just a side effect - it’s a disease accelerator.
This is why pain management in kidney disease isn’t just about picking the right drug. It’s about using opioids as little as possible, for as short as possible, and always with a plan to taper.
What’s Changing in 2025?
Guidelines are evolving. The KDIGO organization is updating its pain management recommendations in 2024, with new data on tapentadol and newer PAMORAs. The NIDDK’s PAIN-CKD study, launched in 2021, is tracking 1,200 patients over five years to see which regimens lead to the best outcomes.
Also, some hospitals are using AI-powered decision tools in their electronic records. Kaiser Permanente reduced inappropriate opioid prescriptions by 47% between 2018 and 2022 using alerts that flag high-risk prescriptions for kidney patients.
Future guidelines may even use genetic testing. People who are CYP2D6 poor metabolizers have over three times the risk of morphine toxicity. If you’re on morphine and your kidney function is low - get tested. It could save your life.
Bottom Line: Safer Pain Management Starts Here
Chronic pain in kidney disease is real. But the old playbook - reach for morphine or oxycodone - is outdated and dangerous. The safest path is simple:
- Start with non-opioid options whenever possible.
- If opioids are needed, choose fentanyl (patch) or buprenorphine.
- Never use morphine, codeine, or meperidine.
- Dose based on GFR - start at 50% of normal if GFR is under 30.
- Use naldemedine for constipation.
- Monitor for neurotoxicity and QT prolongation.
- Taper as soon as pain improves.
There’s no perfect opioid for kidney failure. But there are safe choices - if you know where to look. The goal isn’t just to control pain. It’s to protect the kidneys, the brain, and the heart - all at once.
Andrew Baggley
November 19, 2025 AT 07:01Just don’t start ‘em on high doses. Slow and steady wins the race.
Frank Dahlmeyer
November 20, 2025 AT 16:22Codie Wagers
November 22, 2025 AT 13:31Michael Salmon
November 24, 2025 AT 04:53Derron Vanderpoel
November 25, 2025 AT 12:03Timothy Reed
November 26, 2025 AT 14:07Christopher K
November 27, 2025 AT 00:23harenee hanapi
November 27, 2025 AT 02:59Christopher Robinson
November 28, 2025 AT 14:27Zac Gray
November 29, 2025 AT 23:51