When a woman becomes pregnant, her body changes in ways she might not expect-especially when it comes to thyroid function. If she’s already taking thyroid medication, like levothyroxine, those changes mean her dose likely needs to go up. Not a little. Not later. Immediately. Skipping this step can affect not just her health, but her baby’s brain development too.
Why Thyroid Dose Changes in Pregnancy
Thyroid hormone is critical for fetal development, especially in the first 10 to 12 weeks. Before the baby’s own thyroid starts working, it relies entirely on mom’s supply. If mom’s levels are too low, the baby’s brain doesn’t get enough of what it needs to grow properly. Studies show untreated hypothyroidism during pregnancy can lower a child’s IQ by 7 to 10 points. Worse, it raises the risk of miscarriage and preterm birth.
Here’s the catch: pregnancy increases the body’s demand for thyroid hormone by 30% to 50%. That’s not a guess-it’s backed by data from over 280 women tracked through their pregnancies. Their average levothyroxine dose jumped from 85.7 mcg before pregnancy to 100.0 mcg by the first trimester. That’s a 14.3 mcg increase, on average. For some, it’s more.
When and How to Adjust the Dose
Don’t wait for your next prenatal visit. The moment you find out you’re pregnant, your dose should be adjusted. The American Thyroid Association recommends increasing levothyroxine by 20% to 30% as soon as pregnancy is confirmed. Some experts, like those from ACOG, suggest an even bigger jump: a 50 mcg increase right away for women with pre-existing hypothyroidism.
How do you know how much to increase? It depends on your starting point:
- If your TSH was already high before pregnancy (over 10 mIU/L), start with 1.6 mcg per kg of body weight per day.
- If your TSH was between 5 and 10, increase by 25 to 50 mcg daily.
- If your TSH was over 20, you may need a jump of 75 to 100 mcg.
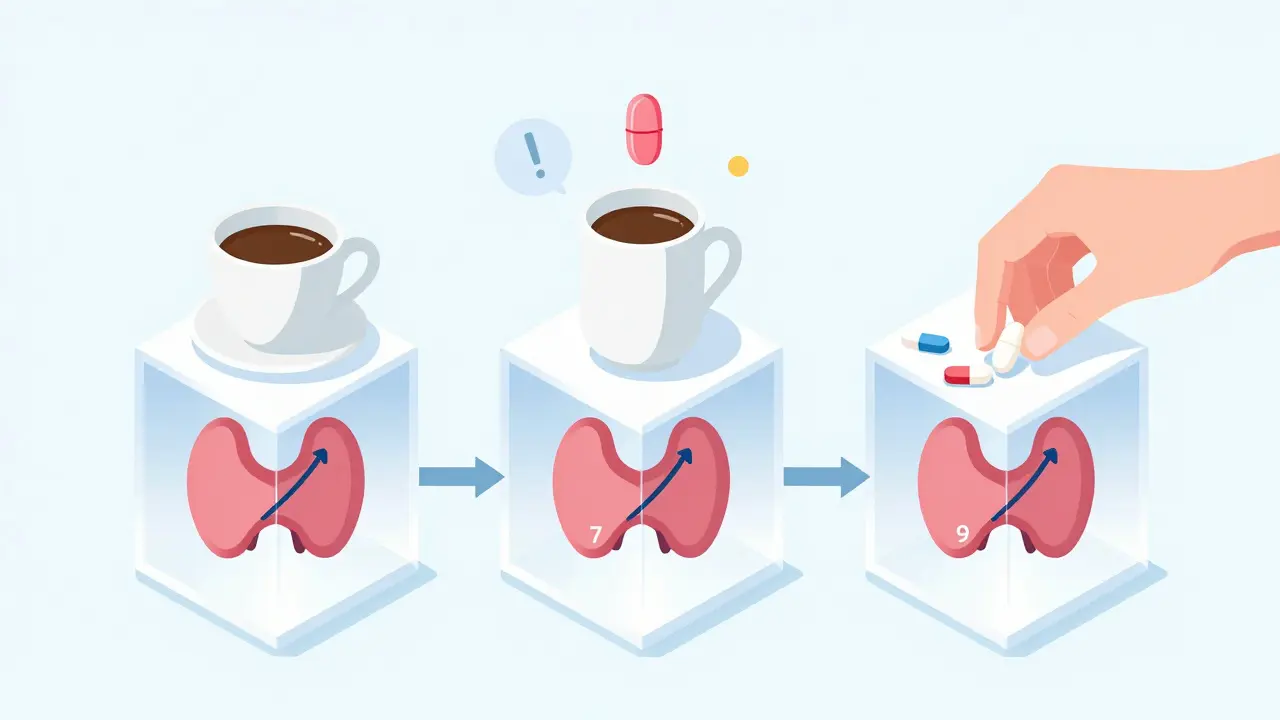
Many women find it easier to take two extra doses per week-so instead of seven pills a week, they take nine. But here’s a common mistake: taking both extra doses on the weekend. That can cause your TSH to spike on Monday morning. Better to space them out: one extra pill every other day.
Monitoring TSH Levels: The Gold Standard
Adjusting the dose is only half the battle. You need to know if it worked. That’s where TSH testing comes in. The American Thyroid Association says check your TSH every four weeks after any dose change-until it stabilizes. The Endocrine Society agrees but adds that the target range shifts slightly by trimester.
Here’s what the numbers mean:
- First trimester: TSH should be ≤ 2.5 mIU/L
- Second and third trimesters: TSH can go up to 3.0 mIU/L
But some experts, like Dr. Peter Laurberg, argue that pushing TSH below 2.5 all the way through might lead to overtreatment. Still, the consensus is clear: if your TSH is above 2.5 in the first trimester, your risk of miscarriage goes up by nearly 70%. That’s why most doctors now err on the side of caution.
Real-world data shows 85% of women with pre-existing hypothyroidism need a dose increase during pregnancy. And 75% of those changes happen in the first trimester alone. If you wait until your 12-week appointment to check your TSH, you’re already behind.
How to Take Your Medication Right
Even if your dose is perfect, it won’t help if you’re not absorbing it. Levothyroxine is sensitive to what you eat and what else you take.
- Take it on an empty stomach-first thing in the morning, 30 to 60 minutes before breakfast.
- Avoid calcium supplements, iron pills, and antacids for at least four hours after taking your dose. These can cut absorption by up to 50%.
- Don’t switch brands without checking with your doctor. While generic levothyroxine is usually fine, some women notice differences when switching from Synthroid® to a generic version.
One patient on a thyroid forum shared: “I took my pill with my morning coffee and a calcium supplement. My TSH jumped from 1.8 to 5.1 in three weeks. I didn’t realize it was the coffee and calcium.”
What Happens If You Don’t Adjust?
Delayed adjustments are common-and dangerous. A survey of 150 OB/GYNs found that 68% didn’t check TSH at the first prenatal visit for women with known thyroid disease. That’s a major gap. Another study showed women whose doses were adjusted within four weeks of pregnancy confirmation had 23% fewer preterm births than those who waited.
And it’s not just about birth outcomes. Children born to mothers with uncontrolled hypothyroidism in early pregnancy are more likely to have lower IQ scores, attention problems, and learning delays. The difference isn’t subtle. It’s measurable. It’s lasting.
Technology and Tools That Help
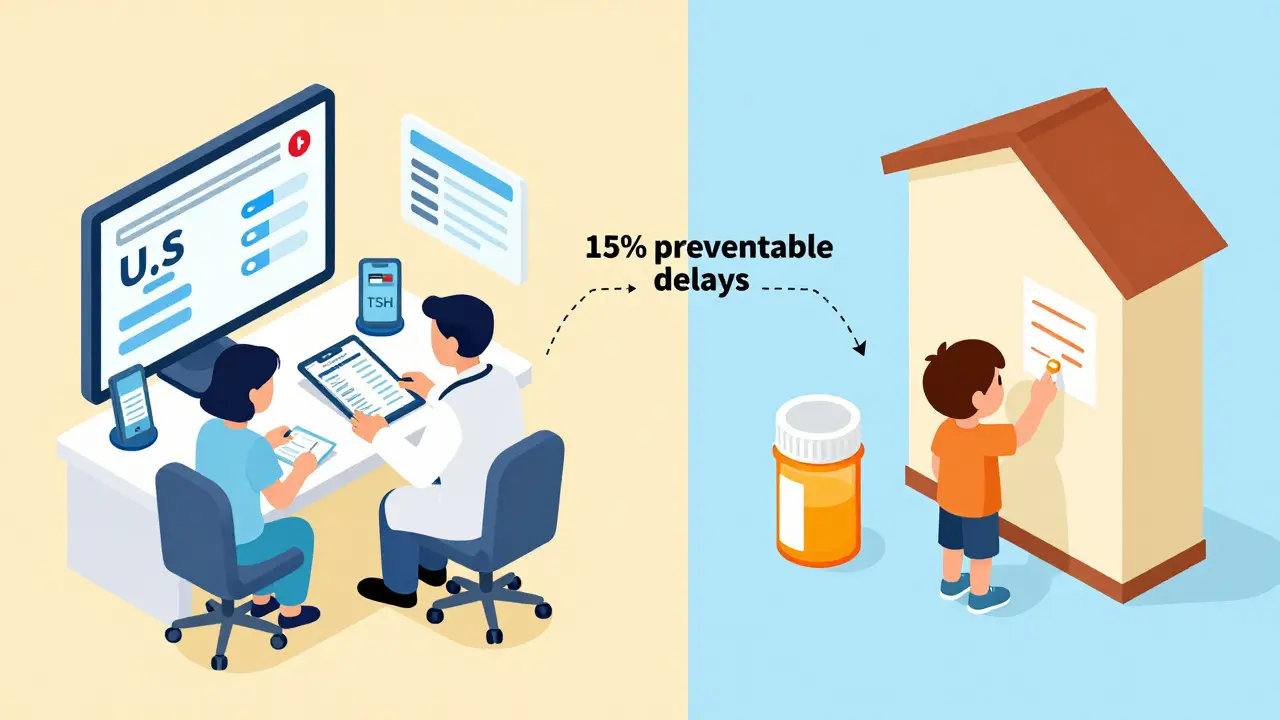
Thankfully, tools are getting better. The MyThyroid app, used by over 12,500 pregnant women since 2019, helps track doses, TSH results, and reminders. 87% of users say it improved their adherence. Hospitals like those using Epic’s EHR system now have automated alerts that pop up when a pregnant patient is on levothyroxine-reminding providers to check TSH and adjust dose.
Even more promising: AI tools are being tested to predict individual dose needs based on pre-pregnancy TSH, weight, and antibody status. One 2022 trial showed these tools improved TSH control by 28% compared to standard dosing. The future is personalized.
Global Gaps and Real-World Challenges
But not everyone has access to these advances. In low-income countries, only 22% have consistent access to levothyroxine. That’s why 15% of preventable developmental delays in children worldwide are tied to untreated maternal hypothyroidism. The WHO added levothyroxine to its Essential Medicines List in 2023-a step toward fixing that gap.
Here’s what you need to do: if you’re on thyroid medication and thinking about pregnancy-or already pregnant-don’t wait. Talk to your doctor now. Get your TSH checked. Adjust your dose. Don’t assume your old dose is still right. Your baby’s brain is counting on it.
Should I increase my levothyroxine dose as soon as I get a positive pregnancy test?
Yes. The majority of experts, including the American Thyroid Association, recommend increasing your dose by 20% to 30% immediately upon confirming pregnancy. Waiting for your first prenatal visit can delay critical hormone support for your baby’s brain development. Many women need this increase even before they know they’re pregnant, since thyroid demand rises right after conception.
How often should TSH be checked during pregnancy?
Check TSH every four weeks after any dose change, and at least once per trimester if stable. Most guidelines recommend testing at 4-6 weeks’ gestation, then again at 16-20 weeks, 24-28 weeks, and 32-34 weeks. This ensures your dose stays on track as your body’s needs change. Don’t wait until your 28-week visit to check-your baby’s development depends on timely adjustments.
Can I take my thyroid medication with food or vitamins?
No. Levothyroxine absorption drops by 35% to 50% if taken with calcium, iron, or antacids. Even coffee, soy, or high-fiber meals can interfere. Take it on an empty stomach, 30 to 60 minutes before eating. If you take supplements, wait at least four hours after your thyroid pill. Consistency matters more than the exact time-so pick a routine and stick to it.
Is it safe to take levothyroxine during pregnancy?
Yes. Levothyroxine is classified as FDA Pregnancy Category A, meaning no evidence of risk in human studies. In fact, it’s safer than not taking it. Untreated hypothyroidism poses far greater risks to both mother and baby than the medication itself. Millions of women have safely taken levothyroxine during pregnancy with excellent outcomes for their children.
What if my TSH is normal but I have thyroid antibodies?
Even if your TSH is normal, the presence of thyroid antibodies (like TPO) increases your risk of developing hypothyroidism during pregnancy. The Endocrine Society recommends treating these women with levothyroxine if TSH is above 2.5 mIU/L in the first trimester, even if they were previously euthyroid. This reduces the risk of miscarriage and developmental delays. Don’t assume normal TSH means no action is needed-antibodies change the game.
Do I need to keep taking thyroid medication after pregnancy?
Yes, but your dose will likely need to be lowered. Most women return to their pre-pregnancy dose within 4 to 8 weeks after delivery. However, some may need to stay on the higher pregnancy dose if their thyroid function doesn’t fully recover. Get your TSH checked 6 to 8 weeks postpartum to confirm the right dose. Breastfeeding is safe with levothyroxine-it doesn’t pass into breast milk in harmful amounts.
Random Guy
February 7, 2026 AT 19:57Brett Pouser
February 8, 2026 AT 18:59Andy Cortez
February 10, 2026 AT 01:47Joseph Charles Colin
February 10, 2026 AT 16:49Chima Ifeanyi
February 11, 2026 AT 15:14Tori Thenazi
February 11, 2026 AT 16:44Jonah Mann
February 13, 2026 AT 15:33THANGAVEL PARASAKTHI
February 15, 2026 AT 05:15Chelsea Deflyss
February 17, 2026 AT 01:39Tricia O'Sullivan
February 18, 2026 AT 12:37Scott Conner
February 19, 2026 AT 06:40