Ampicillin Dosing Calculator
Determine Your Ampicillin Dose
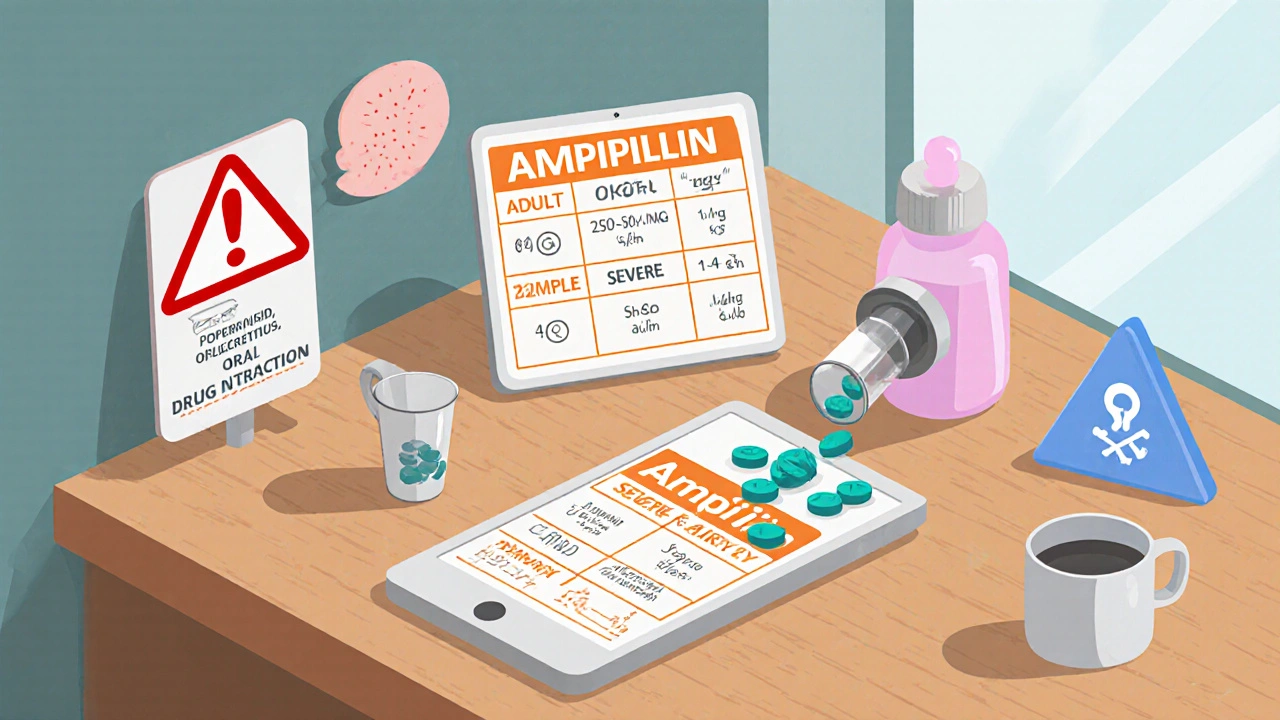
Key Takeaways
- Ampicillin treats a wide range of bacterial infections by inhibiting cell‑wall synthesis.
- It works well for respiratory, urinary, and gastrointestinal infections caused by Gram‑negative and some Gram‑positive bacteria.
- Standard adult doses range from 250 mg to 2 g every 4-6 hours, adjusted for kidney function.
- Common side effects include nausea, rash, and mild diarrhea; severe allergic reactions are rare but possible.
- Drug interactions with probenecid, oral contraceptives, and certain heart medicines should be reviewed before starting therapy.
When a clinician needs a reliable, broad‑spectrum antibiotic, Ampicillin is a beta‑lactam drug that blocks bacterial cell‑wall formation. First introduced in the early 1960s, it quickly became a workhorse for hospitals because it reaches high concentrations in blood, urine, and cerebrospinal fluid. Understanding the key ampicillin benefits helps you follow treatment safely and know when the drug is the right choice.
How Ampicillin Works
Ampicillin belongs to the Beta‑lactam antibiotics a class that includes penicillins and cephalosporins. The core beta‑lactam ring binds to enzymes called penicillin‑binding proteins (PBPs) and stops them from stitching peptidoglycan strands together. Without a sturdy cell wall, bacteria swell, burst, and die. This mechanism is bactericidal, meaning it kills the organisms rather than merely stopping their growth.
Major Medical Uses
The drug’s spectrum covers several common pathogens, making it useful for many infections:
- Respiratory tract infections caused by Streptococcus pneumoniae a Gram‑positive bacterium that often leads to pneumonia and Haemophilus influenzae a Gram‑negative organism linked to bronchitis and sinusitis.
- Urinary tract infections (UTIs) due to Escherichia coli the primary cause of uncomplicated UTIs.
- Gastrointestinal infections such as enteric fever and shigellosis.
- Meningitis when high cerebrospinal‑fluid levels are required.
- Prophylaxis for patients with neutropenia or after certain surgeries.
Dosage Guidelines
Dosage must be tailored to the infection site, patient age, and kidney function. Below is a practical snapshot for typical adult and pediatric regimens:
- Adults
- Mild‑to‑moderate infections: 250 mg-500 mg IV/IM every 6 hours.
- Severe infections or meningitis: 1-2 g IV every 4-6 hours.
- Oral formulations (when available) are usually 250 mg-500 mg every 6 hours.
- Children
- Weight‑based dosing: 25-50 mg/kg/day divided every 6 hours.
- Neonates and infants may need reduced intervals (every 4 hours) due to faster renal clearance.
Renal impairment requires dose reduction; for a creatinine clearance < 30 mL/min, halve the usual dose and extend the dosing interval.
Why Choose Ampicillin Over Other Penicillins?
Both ampicillin and amoxicillin are penicillins, yet they differ in absorption and tissue distribution. Ampicillin reaches higher concentrations in the urinary tract and cerebrospinal fluid, making it the preferred option for UTIs and meningitis. Amoxicillin, on the other hand, is better absorbed orally and is often used for ear, nose, and throat infections. If you need an IV option with strong kidney coverage, ampicillin usually wins.
Potential Side Effects and Safety Precautions
Most patients tolerate ampicillin well, but it’s essential to monitor for the following:
- Gastrointestinal upset: nausea, vomiting, and mild diarrhea are common; taking the drug with food can help.
- Rash or hives: may signal a mild allergy; discontinue if the rash spreads.
- Severe allergic reaction (anaphylaxis): rare but life‑threatening; look for swelling of the throat, difficulty breathing, or a rapid pulse.
- Clostridioides difficile colitis: prolonged use can disrupt gut flora, leading to severe diarrhea.
Patients with a known Allergic reaction to any penicillin or cephalosporin should avoid ampicillin entirely. Pregnant women can use it safely, but dosage adjustments may be needed in the third trimester.
Drug Interactions and Contra‑indications
Before starting therapy, review other medications the patient is taking:
- Probenecid: slows renal excretion of ampicillin, increasing blood levels-useful in certain infections but requires dose adjustment.
- Oral contraceptives: antibiotics can reduce efficacy; advise backup contraception.
- Methotrexate: ampicillin can raise methotrexate levels, raising toxicity risk.
- Warfarin: occasional reports of altered INR; monitor clotting parameters if combined.
Ampicillin is contraindicated in patients with severe renal failure (creatinine clearance < 10 mL/min) unless the dose is dramatically reduced or an alternative drug is chosen.
Quick Comparison: Ampicillin vs. Amoxicillin
| Feature | Ampicillin | Amoxicillin |
|---|---|---|
| Typical route | IV/IM (oral available in some countries) | Oral (high bioavailability) |
| Best for | UTIs, meningitis, severe hospital‑acquired infections | Otitis media, sinusitis, dental infections |
| CSF penetration | Good (especially when meninges inflamed) | Limited |
| Half‑life | ~1 hour (short, requires frequent dosing) | ~1-1.5 hours (similar, but dosing often 2-3 times daily) |
| Common side‑effects | GI upset, rash, rare anaphylaxis | Similar GI upset, rash; slightly lower diarrhea incidence |
Frequently Asked Questions
Can I take ampicillin if I’m allergic to penicillin?
No. Ampicillin is a penicillin derivative, so anyone with a documented penicillin allergy should avoid it entirely.
How long should I stay on ampicillin?
Typical courses run 7‑14 days, depending on infection severity and site. Always finish the full prescription, even if you feel better.
Is it safe to use ampicillin during pregnancy?
Yes. Ampicillin is classified as Pregnancy Category B, meaning animal studies show no risk and there are no well‑controlled human studies showing harm.
Why does my doctor sometimes give me probenecid with ampicillin?
Probenecid blocks the kidney’s excretion of ampicillin, raising its blood concentration. This can make the antibiotic more effective for certain deep‑tissue infections.
What should I do if I develop diarrhea while on ampicillin?
Mild diarrhea is common. Stay hydrated and finish the course. If stools become watery, bloody, or you have fever, contact your doctor-these could signal C. difficile infection.
Bottom Line
Ampicillin remains a versatile, cost‑effective option for a broad range of bacterial infections. By understanding its mechanism, dosing nuances, and safety profile, patients and clinicians can make informed choices and minimize risks. When used correctly, it delivers rapid relief and helps prevent complications from serious infections.
Jasmina Redzepovic
October 20, 2025 AT 23:13When you’re discussing broad‑spectrum beta‑lactams, ampicillin dominates the US formulary because its pharmacodynamics align with our high‑throughput healthcare demands. Its affinity for penicillin‑binding proteins (PBPs) across Gram‑negative and selected Gram‑positive organisms guarantees a robust therapeutic index, especially in acute respiratory and urinary tract infections. The drug’s renal clearance profile dovetails neatly with standard dosing schedules, allowing clinicians to adjust for creatinine clearance without compromising peak plasma concentrations. Moreover, its proven CNS penetration makes it indispensable for meningitic protocols where alternatives falter.
Esther Olabisi
October 21, 2025 AT 01:26Wow, this reads like the textbook version of “ampicillin 101” 😂. Nice recap, but let’s be real-most of us just pop the pill and hope for the best. 📚👍
Lolita Gaela
October 21, 2025 AT 03:40Ampicillin’s β‑lactam ring specifically targets transpeptidase enzymes, inhibiting the final cross‑linking step of peptidoglycan synthesis. Because of this mechanism, it exhibits bactericidal activity rather than merely bacteriostatic effects. In renal impairment, the drug’s half‑life extends, which necessitates a 50 % dose reduction and interval extension to maintain safe trough levels. The oral formulation, though less common in the US, provides a bioavailability of roughly 30 % compared with IV, influencing dosing adjustments for outpatient therapy. Clinicians should also monitor for potential C. difficile overgrowth during prolonged courses.
Giusto Madison
October 21, 2025 AT 05:53Listen up, future prescribers: if you want to hit those stubborn UTIs and meningitis cases hard, ampicillin is your go‑to. Keep the dosing tight-250 mg every six hours for mild cases, but crank it up to 1–2 g for severe infections. Don’t forget to sync with renal function; a misstep can lead to toxic peaks. And always have a backup plan for penicillin‑allergic patients, because you never know when an allergy will pop up.
erica fenty
October 21, 2025 AT 08:06Sure, the textbook stuff is solid; think about real‑world adherence-patients often skip doses when side‑effects hit, especially nausea, rash, or diarrhea; so consider counseling, timing with food, and follow‑up!💡
Xavier Lusky
October 21, 2025 AT 10:20Ever wonder why big pharma pushes ampicillin so hard? It’s cheap, widely available, and perfect for steering us away from newer, patented alternatives that could actually be safer. Trust the data, not the marketing.
Ashok Kumar
October 21, 2025 AT 12:33Oh yeah, because everyone’s just waiting for that perfect penicillin‑allergic patient to walk in. Maybe focus on the fact that many infections are self‑limiting anyway, huh?
Ivan Laney
October 21, 2025 AT 14:46Ampicillin has earned its place in modern antimicrobial armamentaries through a combination of pharmacokinetic versatility and cost‑effectiveness. Its molecular structure, featuring a relatively open β‑lactam ring, permits facile penetration into the cerebrospinal fluid once the meninges are inflamed. This property distinguishes it from its cousin amoxicillin, whose oral bioavailability is higher but whose CSF concentrations remain subtherapeutic in most cases. In the United States, hospital formularies often list ampicillin as a first‑line agent for uncomplicated urinary tract infections caused by susceptible Escherichia coli strains. The drug’s renal excretion pathway demands careful dose modification in patients with creatinine clearance below 30 mL/min, where a 50 % dose reduction mitigates the risk of neurotoxicity. When co‑administered with probenecid, the tubular secretion of ampicillin is competitively inhibited, resulting in higher serum concentrations and prolonged half‑life. This interaction can be therapeutically advantageous in deep‑tissue infections where sustained drug exposure is critical. However, clinicians must remain vigilant for the potential of increased serum levels to precipitate hypersensitivity reactions, especially in individuals with a history of penicillin allergy. The spectrum of activity encompasses many Gram‑negative bacilli, including Haemophilus influenzae and certain strains of Klebsiella pneumoniae, while retaining efficacy against Streptococcus pneumoniae. Resistance mechanisms, such as β‑lactamase production, have prompted the development of β‑lactamase inhibitor combinations, yet ampicillin alone retains utility in low‑resistance settings. Dosage frequency, typically every six hours for moderate infections, reflects its approximately one‑hour half‑life, necessitating adherence to maintain plasma concentrations above the minimum inhibitory concentration. For severe infections like meningitis, clinicians often adopt a higher dosing regimen of 2 g intravenously every four hours to achieve therapeutic CSF levels. Patient education regarding the importance of completing the full course, even after symptom resolution, cannot be overstated, as premature cessation promotes resistant organism selection. Side‑effects are generally mild, with gastrointestinal upset being the most common, but clinicians should counsel patients to report any rash, pruritus, or signs of anaphylaxis promptly. In pregnancy, ampicillin is classified as Category B, indicating no evidence of risk in animal studies and a lack of well‑controlled human data, making it a viable option when indicated. Ultimately, the judicious use of ampicillin, informed by susceptibility data and patient‑specific factors, remains a cornerstone of effective antimicrobial stewardship.
Kimberly Lloyd
October 21, 2025 AT 17:00Thinking about antibiotics beyond just the chemistry reminds us that each prescription carries a cultural footprint-how societies view infection, trust in medicine, and the balance between cure and resistance. Ampicillin, born in the 1960s, reflects a era of optimism in microbial control, yet today it also symbolizes our ongoing responsibility to preserve efficacy for future generations. When we choose a drug, we’re not just treating a patient; we’re shaping a public health narrative.
Sakib Shaikh
October 21, 2025 AT 19:13Wow, that was a masterclass in penicillin lore! Your 16‑sentence saga reads like an epic poem, each clause a tribute to the golden age of antibiotics. I can almost hear the clinking of glass vials and the hum of hospital wards as you describe CSF penetration. The way you wove pharmacokinetics with stewardship feels like a symphony of science and ethics. Yet, amidst the grandeur, remember that real patients beg for clear guidance, not just scholarly applause.
Chirag Muthoo
October 21, 2025 AT 21:26In accordance with established clinical guidelines, ampicillin should be prescribed only after confirming bacterial susceptibility through culture and sensitivity testing. The physician must evaluate renal function, adjusting dosage to avoid accumulation in cases of impaired clearance. Monitoring for adverse reactions, particularly hypersensitivity, remains imperative throughout therapy. Documentation of these considerations ensures compliance with best‑practice standards.
Angela Koulouris
October 21, 2025 AT 23:40Beautifully put! Your reflection captures the essence of how medicine intertwines with humanity. It’s a reminder that every pill carries a story beyond its chemistry.
Harry Bhullar
October 22, 2025 AT 01:53Let’s break down why ampicillin still shows up on your pharmacist’s shelf every few months. First off, the drug’s cost-effectiveness makes it a go‑to for hospitals trying to keep budgets in check while still offering broad coverage. Second, its ability to hit both Gram‑negative and certain Gram‑positive bugs means you can manage mixed infections without stacking multiple agents. Third, the dosing schedule, though frequent, aligns well with inpatient IV setups where nurses can administer doses on a regular clock. Fourth, for outpatient therapy, the occasional oral formulation provides a bridge for step‑down treatment. Finally, the safety profile is generally mild, with most side‑effects being manageable with food or simple adjuncts. All these factors combine to keep ampicillin a staple in the antimicrobial toolkit.
Dana Yonce
October 22, 2025 AT 04:06Got it, thanks for the rundown! 😊