Why Blood Pressure Matters in Kidney Disease
High blood pressure doesn’t just strain your heart-it’s one of the biggest threats to your kidneys. When your kidneys are damaged, they lose the ability to filter waste and control fluid balance. That causes blood pressure to rise, which then damages the kidneys even more. It’s a cycle: high blood pressure hurts the kidneys, and hurt kidneys make blood pressure worse.
For people with chronic kidney disease (CKD), especially those with protein in their urine (albuminuria), controlling blood pressure isn’t just about feeling better. It’s about stopping the damage before it leads to dialysis or a transplant. That’s where ACE inhibitors and ARBs come in. These aren’t just regular blood pressure pills. They’re the only class of antihypertensive drugs proven to slow kidney decline in people with CKD.
How ACE Inhibitors and ARBs Work Differently
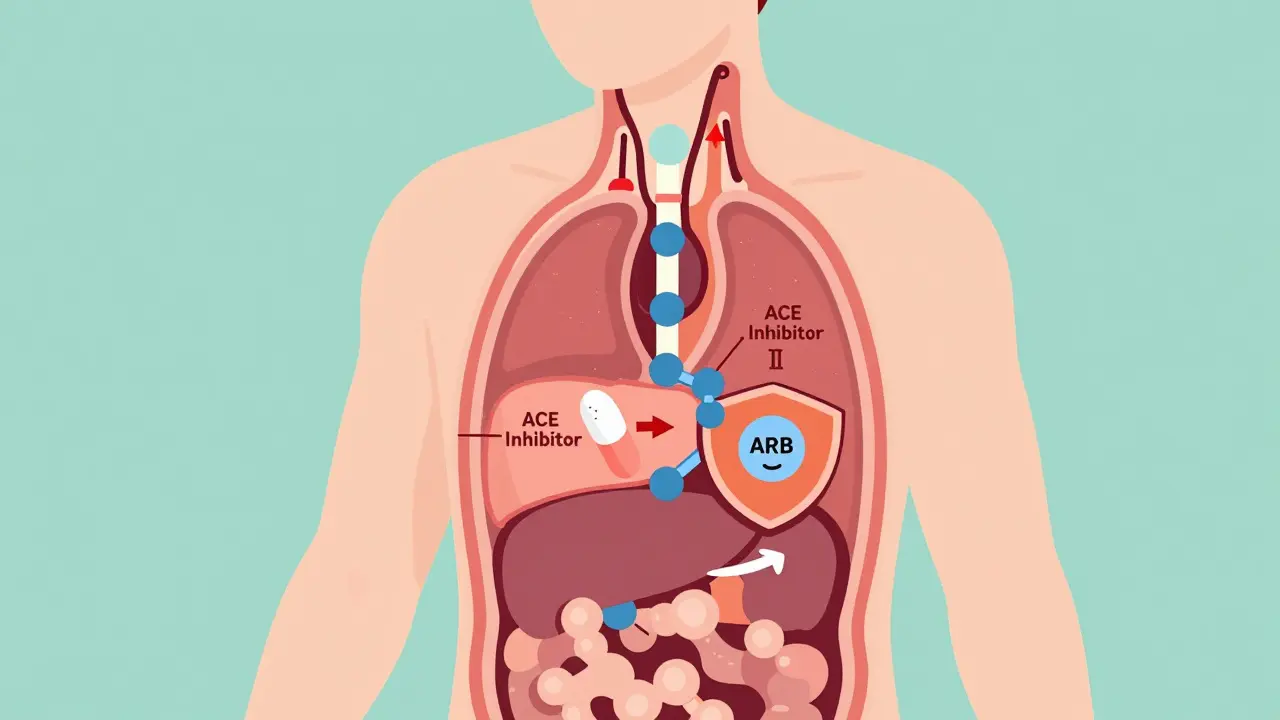
Both ACE inhibitors and ARBs target the same system: the renin-angiotensin-aldosterone system, or RAAS. This system is like a hormone chain reaction that tightens blood vessels and makes your body hold onto salt and water-both of which raise blood pressure.
ACE inhibitors, like lisinopril and enalapril, block the enzyme that turns angiotensin I into angiotensin II. Less angiotensin II means looser blood vessels and less pressure inside the kidney’s filtering units, called glomeruli. ARBs, like losartan and valsartan, don’t block the enzyme. Instead, they block the receptor that angiotensin II binds to. Same result: lower pressure, less strain on the kidneys.
The key difference? Side effects. About 1 in 5 people on ACE inhibitors develop a dry, nagging cough. It’s not dangerous, but it’s annoying enough that many stop taking the pill. ARBs rarely cause this. If you’ve had a cough on an ACE inhibitor, switching to an ARB often fixes it without losing protection.
What the Evidence Shows: Real Benefits, Not Just Theory
Studies from the last 20 years consistently show these drugs do more than lower numbers on a monitor. In people with CKD and proteinuria, ACE inhibitors and ARBs reduce protein loss in urine by 30% to 50%. That’s huge-protein in urine is a direct sign of kidney damage. Less protein means slower decline.
They also cut the risk of kidney failure by 20% to 40%. A 2024 study tracking over 1,200 patients with advanced CKD (eGFR under 20) found those who stayed on ACE inhibitors or ARBs had a 34% lower chance of needing dialysis or a transplant compared to those who switched to other blood pressure meds. That’s not a small edge. That’s life-changing.
And here’s something many doctors still don’t tell patients: you don’t have to stop these drugs just because your kidneys are failing. The old belief was, “If your eGFR drops, stop the pill.” But newer data shows the opposite. Stopping them in stage 4 or 5 CKD may actually speed up kidney decline. The 2023 KDIGO guidelines now say: keep them going, as long as potassium stays below 5.0 mmol/L and your eGFR doesn’t crash by more than 30%.
When to Start-and When to Worry
You don’t need to wait until your kidneys are badly damaged to start. If you have CKD and your urine test shows albumin-to-creatinine ratio above 200 mg/g, guidelines say you should be on one of these drugs. That’s true even if your blood pressure is normal. The protection isn’t just from lowering pressure-it’s direct kidney shielding.
But you can’t just start and forget. Before you begin, your doctor should check your eGFR and potassium level. Then, 1 to 2 weeks after starting or changing the dose, you need a repeat blood test. Why? Because these drugs can cause two predictable issues:
- A temporary dip in eGFR (up to 30%) is normal and often a sign the drug is working. If it drops more than that, your doctor may pause and reassess.
- High potassium (hyperkalemia) happens in 10% to 15% of users. It’s not rare. If your potassium hits 5.5 or higher, you’ll need to adjust your diet, reduce the dose, or switch meds.
Don’t panic if your numbers shift a little. But don’t ignore them, either. Most problems come from not checking at all.
Why So Many People Aren’t Taking Them
Despite strong evidence, only about 58% of patients with advanced CKD are on an ACE inhibitor or ARB. In early-stage CKD, it’s 82%. Why the drop-off?
One reason is fear. Doctors worry about high potassium or sudden kidney function drops. But studies show the risks are manageable with monitoring. Another reason? Misinformation. Some patients stop because they heard these drugs “hurt the kidneys.” The truth? They protect them. Stopping them often makes things worse.
Then there’s the cough. If you’re on lisinopril and can’t sleep because of a dry throat, you’re not alone. But you don’t have to live with it. Switching to an ARB like losartan or irbesartan usually solves it. Same protection. No cough.
And don’t fall for the myth that combining ACE inhibitors and ARBs gives you double the benefit. The VA Nephropathy Trial showed that while dual therapy cuts proteinuria a bit more, it also doubles the risk of acute kidney injury and raises potassium dangerously. No major guideline recommends this combo anymore.

What’s Next? The Future of Kidney Protection
Research is moving beyond ACE inhibitors and ARBs. New drugs like sacubitril/valsartan (Entresto), originally made for heart failure, are now being studied for kidney protection. The 2024 PARADIGM-HF extension found it slowed kidney decline by 22% compared to enalapril in patients with both heart failure and CKD. That’s promising.
But for now, ACE inhibitors and ARBs are still the gold standard. They’re cheap, generic, and backed by decades of data. Losartan and lisinopril are among the top two most prescribed blood pressure pills in the U.S., with over 200 million prescriptions in 2023 alone. That’s not because they’re trendy. It’s because they work.
Real Talk: What Patients Are Saying
On patient forums, stories vary. One man in Sydney, 68, with type 2 diabetes and stage 3 CKD, says he’s been on lisinopril for 8 years. His proteinuria dropped from 800 mg/g to 180 mg/g. His eGFR stayed steady at 45. “I check my potassium every three months. That’s it. I feel fine,” he posted.
Another woman, 55, stopped her ARB after her potassium spiked to 5.8. She was scared. But after switching to a potassium-lowering diet and restarting the same drug at a lower dose, her levels stabilized. “I didn’t realize I could still take it,” she wrote. “I thought I had to quit forever.”
These aren’t rare cases. They’re the norm. The key isn’t avoiding the drugs-it’s managing them wisely.
Bottom Line: Don’t Fear the Pill-Fear the Silence
If you have kidney disease and high blood pressure-or even just protein in your urine-ACE inhibitors and ARBs are your best defense. They’re not perfect. They need monitoring. They can cause side effects. But the alternative-doing nothing or switching to other blood pressure pills-is far riskier.
Ask your doctor: “Am I on the right medicine for my kidneys?” If you’re not, ask why. If you’re on one and stopped because of a cough or a scary lab result, ask if you can try again. The evidence is clear: these drugs save kidneys. You just need to use them right.
Samyak Shertok
January 17, 2026 AT 08:55Travis Craw
January 18, 2026 AT 01:38Christina Bilotti
January 19, 2026 AT 12:17vivek kumar
January 19, 2026 AT 21:11Rob Deneke
January 21, 2026 AT 11:48evelyn wellding
January 23, 2026 AT 02:27Chelsea Harton
January 23, 2026 AT 07:49Corey Chrisinger
January 24, 2026 AT 17:28Bianca Leonhardt
January 26, 2026 AT 08:43brooke wright
January 27, 2026 AT 10:43Nick Cole
January 28, 2026 AT 20:16Riya Katyal
January 29, 2026 AT 19:41Henry Ip
January 30, 2026 AT 13:59