Deflazacort Interaction Checker
Check Your Medications
Enter the medications you're currently taking to see if they interact with Deflazacort.
Interaction Results
When you see Deflazacort is a synthetic corticosteroid prescribed for conditions like Duchenne muscular dystrophy, rheumatoid arthritis, and asthma, the first question is usually “Will it play nice with my other meds?” The short answer: sometimes, but not always. This guide breaks down the most common deflazacort drug interactions, explains why they happen, and gives you practical steps to stay safe.
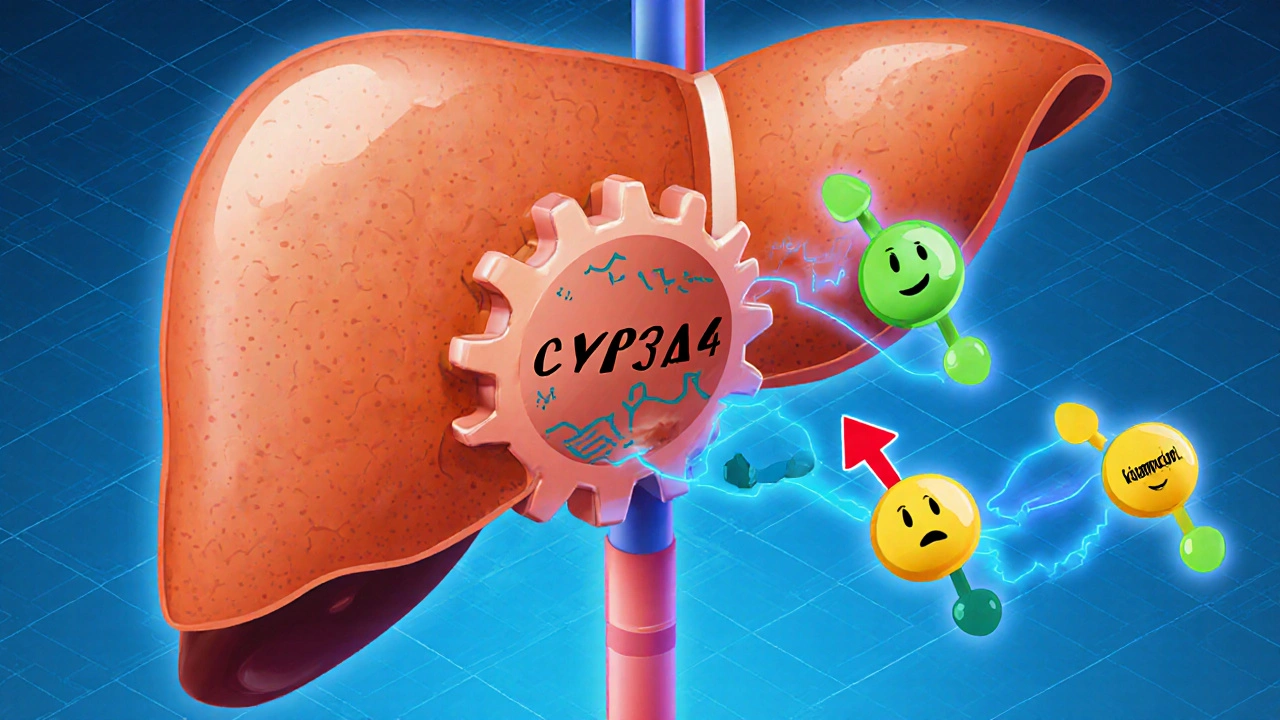
How Deflazacort Works in the Body
Deflazacort belongs to the Corticosteroids family. It reduces inflammation by binding to glucocorticoid receptors, which then suppress the transcription of pro‑inflammatory genes. Because it’s metabolized mainly by the liver enzyme CYP3A4, anything that speeds up or slows down this enzyme can change how much drug ends up in your bloodstream.
Why Drug Interactions Matter
Even a modest shift in deflazacort levels can tip the balance between therapeutic benefit and side‑effects. Too much exposure may raise the risk of elevated blood glucose, bone loss, or severe infections. Too little, and the inflammation you’re trying to control can flare up again. That’s why knowing which drugs - or even foods and supplements - interact with deflazacort is essential for anyone on a long‑term regimen.
Enzyme Inhibitors and Inducers (The CYP3A4 Story)
Medications that block CYP3A4 raise deflazacort concentrations; those that boost the enzyme lower them. Below are the most frequent culprits.
- Azithromycin - a macrolide antibiotic that weakly inhibits CYP3A4. When taken together, patients have reported a 20‑30% rise in corticosteroid side‑effects.
- Ketoconazole and other strong antifungals - can double deflazacort levels, demanding dose cuts.
- Rifampicin - a potent inducer that may cut deflazacort exposure by up to 50%, potentially causing loss of disease control.
Anticoagulants and Bleeding Risk
Deflazacort can enhance the effects of blood thinners by affecting clotting factor synthesis. The classic example is Warfarin.
Studies from 2022 showed that patients on both drugs experienced an average INR increase of 0.5 to 1.0 units, raising the chance of minor bleeding. Regular INR monitoring and possibly a lower warfarin dose are advised.
NSAIDs and Gastrointestinal Safety
Non‑steroidal anti‑inflammatory drugs (NSAIDs) like Ibuprofen add to the stomach‑lining irritation already possible with corticosteroids.
Combined use has been linked to a two‑fold rise in gastric ulcer risk. If you need pain relief, consider acetaminophen or a proton‑pump inhibitor for protection.
Impact on Blood Sugar and Diabetes Management
Corticosteroids raise blood glucose by stimulating gluconeogenesis. When paired with oral hypoglycemics (e.g., metformin) or insulin, you may need tighter glucose monitoring and dose adjustments.
In a 2021 cohort of 150 patients with type 2 diabetes, those on deflazacort saw an average HbA1c increase of 0.7 % over three months if their diabetes meds were unchanged.
Bone Health Concerns
Long‑term corticosteroid exposure can reduce bone mineral density (BMD), especially when combined with drugs that also affect calcium metabolism, such as certain anticonvulsants (e.g., phenytoin).
Doctors often prescribe calcium, vitamin D, or bisphosphonates to counteract this effect.
Vaccines and Immune Response
Deflazacort suppresses the immune system, which may blunt the response to live vaccines (e.g., varicella, measles). The recommendation is to delay live vaccines until the steroid dose falls below 0.5 mg/kg/day or to use inactivated alternatives when possible.
Managing Interactions: A Practical Toolkit
Here’s a step‑by‑step plan you can follow whenever a new medication is added to your regimen.
- Check if the new drug is a known CYP3A4 inhibitor or inducer.
- Ask your pharmacist to review the full medication list for anticoagulant, NSAID, or antidiabetic overlap.
- Request baseline labs - INR for warfarin, fasting glucose for diabetics, and a DEXA scan for bone density if you’re on long‑term therapy.
- Adjust the deflazacort dose if needed (usually 20‑30% reduction for strong inhibitors, 25‑50% increase for strong inducers).
- Schedule follow‑up labs within 1‑2 weeks of any change.
- Document every adjustment in a medication diary or digital app.
Interaction Severity at a Glance
| Interacting drug | Mechanism | Severity | Clinical tip |
|---|---|---|---|
| Azithromycin | CYP3A4 inhibition | Moderate | Consider 20 % dose reduction |
| Rifampicin | CYP3A4 induction | High | Increase deflazacort dose or switch steroid |
| Warfarin | Altered clotting factor synthesis | Moderate | Check INR twice weekly after start |
| Ibuprofen | Gastro‑intestinal irritation | Low‑to‑moderate | Add PPI or use acetaminophen |
| Metformin | Blood‑glucose elevation | Low | Monitor fasting glucose, adjust metformin if needed |
Quick Interaction Checklist
- Is the new drug a CYP3A4 inhibitor (e.g., azithromycin, ketoconazole)? → Reduce deflazacort dose.
- Is it a CYP3A4 inducer (e.g., rifampicin, carbamazepine)? → Increase dose or consider an alternative steroid.
- Will it increase bleeding risk (e.g., warfarin, aspirin)? → Monitor INR or clotting parameters.
- Does it irritate the gut (e.g., ibuprofen, naproxen)? → Use gastric protectors or switch pain reliever.
- Can it raise blood sugar (e.g., high‑dose steroids, certain diuretics)? → Check glucose more often.
- Is bone health a concern? → Add calcium/vitamin D, consider bisphosphonate.
When to Call Your Healthcare Provider
If you notice any of the following while on deflazacort, seek advice promptly:
- Unexplained bruising or bleeding.
- Severe stomach pain or black stools.
- Sudden rise in blood sugar readings.
- Joint pain or fractures with minimal trauma.
- Signs of infection (fever, persistent cough).
Frequently Asked Questions
Can I take over‑the‑counter cold medicine with deflazacort?
Most decongestants (like pseudoephedrine) are safe, but avoid multi‑symptom formulas that contain NSAIDs. Choose a product with only antihistamines or a simple saline rinse.
Do herbal supplements interact with deflazacort?
St. John’s wort is a strong CYP3A4 inducer and can lower steroid levels, risking disease flare. Ginkgo, garlic, and ginseng can also affect clotting, so discuss any supplement with your pharmacist.
Is it safe to take vitamin D supplements while on deflazacort?
Yes-vitamin D actually helps counteract steroid‑induced bone loss. A daily dose of 800‑1000 IU is commonly recommended, but your doctor may adjust based on blood levels.
How long does it take for an interaction to show up?
Enzyme‑based changes can appear within a few days, while effects on blood sugar or bone density may take weeks to months. Regular monitoring catches problems early.
Should I stop deflazacort before surgery?
Most surgeons advise tapering the dose gradually to reduce infection risk and aid wound healing. Speak with your prescribing doctor at least two weeks ahead of any planned operation.
Bottom Line
Deflazacort is a powerful tool, but like any medication, it doesn’t live in isolation. By spotting enzyme interactions, watching for bleeding or blood‑sugar spikes, and keeping bone health on the radar, you can stay ahead of side‑effects and keep your primary condition under control.
Dante Russello
October 23, 2025 AT 18:04When you add a new med, always scan the label for CYP3A4 clues, because those enzymes decide how much deflazacort hangs around in your blood; a hidden inhibitor can push levels upward, a silent inducer can pull them down, and the side‑effects follow accordingly, so a quick pharmacist check is worth the extra minute, especially with antibiotics like azithromycin or antifungals such as ketoconazole; remember, the liver’s busy, and the more you load it, the more unpredictable the steroid’s journey becomes, which is why a medication list on your phone helps keep the doctor in the loop, plus it prevents accidental combos that could spike glucose or thin your blood.
James Gray
November 4, 2025 AT 06:50Yo, just a heads up – if you’re popping any over‑the‑counter cold stuff, steer clear of the ones that sneak in ibuprofen; stick to plain decongestants or antihistamine combos, they’re less likely to mess with your stomach or steroid levels – keep it chill and you’ll dodge the ulcer drama.
Scott Ring
November 15, 2025 AT 20:37Quick tip: always let your doc know if you start a new vitamin, especially high‑dose vitamin D, because it can actually support bone health while you’re on deflazacort, and it won’t interfere with the steroid’s metabolism – just a friendly reminder to add it to your med list.
Shubhi Sahni
November 27, 2025 AT 10:24Don’t forget that St. John’s wort is a potent CYP3A4 inducer – it can shave off half the effectiveness of deflazacort, leading to flare‑ups, so if you’re taking that herb, have a conversation with your pharmacist; similarly, garlic and ginkgo may play with clotting, which matters if you’re on warfarin.
Danielle St. Marie
December 9, 2025 AT 00:10Honestly, if you’re still trusting folk‑medicine over evidence‑based care, you’re asking for trouble – these interactions aren’t a rumor, they’re documented, so stop the nonsense and get a proper review 🙄💥.
Peter Richmond
December 20, 2025 AT 13:57Adjust the dose by 20 % when adding a strong CYP3A4 inhibitor; increase by 30 % with a known inducer.
Bonnie Lin
January 1, 2026 AT 03:44Always keep a written list of all meds and supplements you take.
sara fanisha
January 12, 2026 AT 17:30Stay on top of your blood sugar checks if you’re diabetic – steroids can push numbers up fast.
Jinny Shin
January 24, 2026 AT 07:17Picture this: you’re juggling deflazacort, a new antibiotic, and a night out, when suddenly your INR spikes – the drama of a bleeding episode could have been avoided with a simple lab check, so don’t let the plot twist catch you off guard.
Mike Peuerböck
February 4, 2026 AT 21:04When a patient starts rifampicin, the enzyme induction can slash deflazacort levels dramatically, sometimes by as much as half, which means the anti‑inflammatory shield weakens and disease activity may rebound; clinicians should anticipate this shift and either boost the steroid dose or consider switching to a corticosteroid less reliant on CYP3A4 metabolism; the same principle applies to strong inducers like carbamazepine, where a careful titration schedule can stave off a flare; on the flip side, strong inhibitors such as ketoconazole demand a dose reduction of roughly 30‑40 % to keep side‑effects like hyperglycaemia and bone loss in check; this balancing act is not just a pharmacokinetic curiosity but a real‑world necessity that protects patients from avoidable complications; regular monitoring of glucose, INR, and bone density becomes essential during any medication change, providing objective data to guide dose adjustments; blood work should be ordered within one to two weeks of adding or removing a known interacting drug, allowing time for steady‑state levels to settle; pharmacists play a pivotal role, often catching interactions that physicians may overlook in a busy clinic; they can recommend alternative agents or suggest timing strategies that minimize overlap; patients should be educated to report new symptoms promptly, such as unexplained bruising, abdominal pain, or persistent hyperglycaemia, as these may signal an interaction gone awry; a comprehensive medication diary, whether paper‑based or digital, serves as a safety net, ensuring every ingredient is accounted for; finally, interdisciplinary communication-between primary care, specialists, and pharmacy-creates a robust safety net, reducing the risk of adverse events and preserving therapeutic efficacy.
Simon Waters
February 16, 2026 AT 10:50If you take any new drug, check if it is a CYP3A4 inducer or inhibitor; this can change the steroid level.
Vikas Kumar
February 28, 2026 AT 00:37Never trust the system when it downplays the danger of mixing steroids with blood thinners; the hidden risks are real and can turn a routine checkup into a nightmare.