When you’re managing diabetes, taking the right meds can mean the difference between steady blood sugar and a medical emergency. But what many people don’t realize is that diabetes drug interactions can turn a safe treatment plan into a dangerous one. Some combinations boost blood sugar too high. Others crash it too low-sometimes without warning. The stakes are real: hypoglycemia can lead to seizures, falls, or even coma. Hyperglycemia can trigger long-term damage to kidneys, nerves, and eyes. And it’s not just about your diabetes pills. It’s what you’re taking alongside them-antibiotics, heart meds, even over-the-counter painkillers.
Why Some Diabetes Drugs Clash
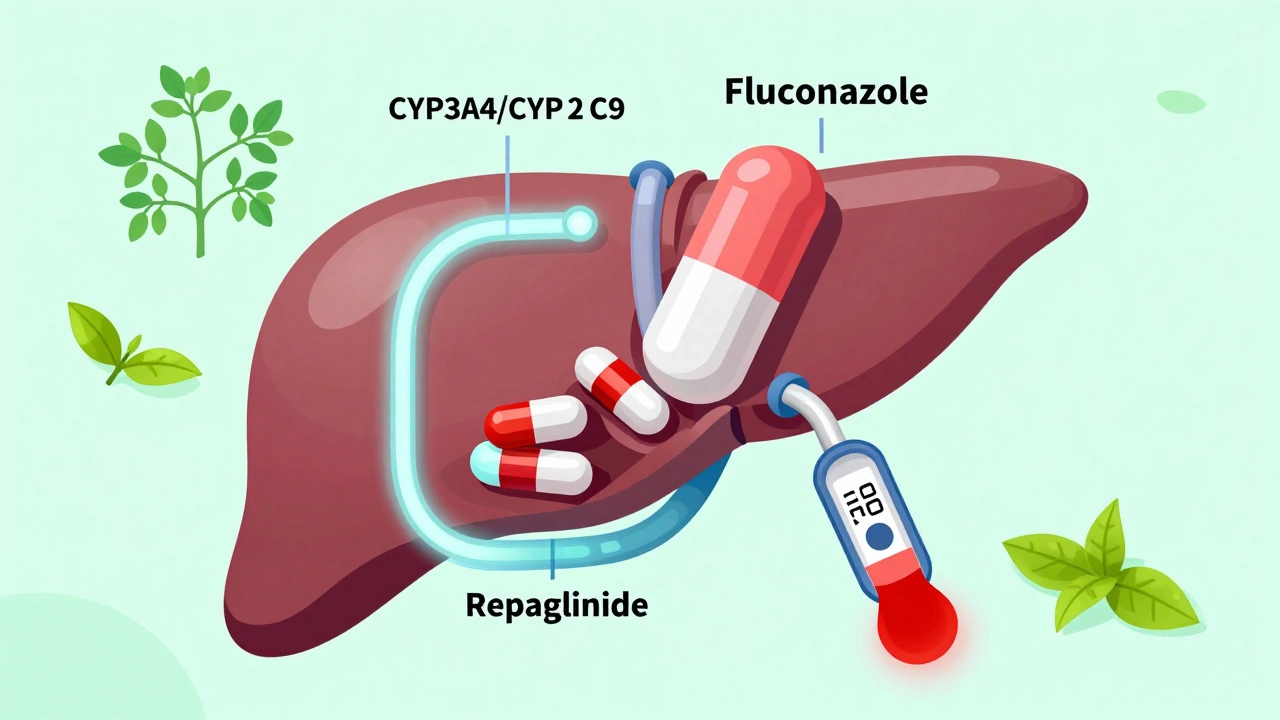
Not all diabetes medications work the same way. Some stimulate your pancreas to release more insulin. Others help your body use insulin better. A few make your kidneys flush out extra sugar. When two drugs with similar effects are mixed, they can pile up too much insulin in your system. That’s how you get dangerously low blood sugar. Other drugs interfere with how your liver or kidneys process your diabetes meds. This changes how long they last-or how strong they become.One of the biggest culprits is the CYP450 enzyme system. Your liver uses enzymes like CYP3A4 and CYP2C9 to break down drugs. If another medication blocks those enzymes-like the antifungal ketoconazole or the antibiotic clarithromycin-your diabetes drug doesn’t get cleared from your body. It builds up. That’s why repaglinide and nateglinide, two fast-acting insulin secretagogues, are especially risky when paired with these drugs. Studies show blood sugar can drop below 40 mg/dL within hours. That’s not a spike. That’s a crash.
High-Risk Combinations to Watch Out For
- Insulin + Rosiglitazone: Rosiglitazone (Avandia) helps your body respond better to insulin. But when combined with insulin itself, it can cause severe fluid retention. This leads to swelling in the legs and, in worst cases, heart failure. The American Diabetes Association warns against this combo, especially in older adults or those with existing heart conditions.
- Meglitinides + Azole Antifungals: Drugs like ketoconazole, itraconazole, or fluconazole block CYP3A4 and CYP2C8. Since repaglinide and nateglinide rely on these enzymes to break down, the result is prolonged insulin release. A single dose of fluconazole can turn a normal mealtime dose into a 12-hour hypoglycemia risk.
- Metformin + Contrast Dye: If you’re scheduled for a CT scan or angiogram, your doctor may tell you to stop metformin for 48 hours. Why? The contrast dye can temporarily reduce kidney function. Metformin is cleared by the kidneys. If they slow down, metformin builds up and can cause lactic acidosis-a rare but deadly condition.
- DPP-4 Inhibitors + GLP-1 RAs: Sitagliptin, linagliptin, saxagliptin-all DPP-4 inhibitors-work by keeping your body’s natural GLP-1 hormone active. GLP-1 receptor agonists like semaglutide or liraglutide do the same thing, but stronger. Combining them doesn’t make blood sugar control better. It just increases side effects like nausea and pancreatitis risk. The ADA explicitly says this combo is unnecessary and should be avoided.
- Diabetes Meds + Corticosteroids: Prednisone, dexamethasone, even inhaled steroids can spike blood sugar. If you’re on insulin or sulfonylureas and start a steroid course, your glucose levels can jump 100-200 mg/dL. You’ll need a temporary dose adjustment. Waiting until your sugar hits 300 mg/dL is too late.
Why GLP-1 RAs and SGLT-2 Inhibitors Are Safer Partners
The newer class of diabetes drugs-GLP-1 receptor agonists and SGLT-2 inhibitors-have become favorites not just because they help with weight loss and heart protection. They also play nicely with other meds. GLP-1 RAs like semaglutide don’t rely on liver enzymes the way older drugs do. They’re cleared slowly through the kidneys and broken down by common proteins, not CYP450. That means fewer interactions. Same with SGLT-2 inhibitors like empagliflozin or dapagliflozin. They work directly in the kidneys to push sugar out in urine. Their pathway is mostly independent of other drugs.This is why guidelines now recommend GLP-1 RA + insulin over insulin alone. The combo gives better A1C control, less weight gain, and fewer low-blood-sugar episodes. A 2024 study in The Lancet Diabetes & Endocrinology found that patients on semaglutide plus insulin had 40% fewer hypoglycemic events than those on insulin alone. That’s not just a small win. It’s life-changing.
Hidden Risks: Over-the-Counter and Herbal Products
You might think only prescription drugs matter. But that’s not true. Many people take herbal supplements or OTC meds without telling their doctor. And that’s where things go wrong.- St. John’s Wort: This popular herb for mood support boosts CYP3A4 activity. That means it speeds up the breakdown of sulfonylureas like glimepiride. Your blood sugar rises because the drug doesn’t last as long.
- Green Tea Extract: High doses can inhibit CYP2C9, the same enzyme that breaks down nateglinide. This can lead to unexpected hypoglycemia, especially in people taking it with other meds.
- Quinine: Found in some leg cramp remedies and tonic water, quinine can trigger hypoglycemia on its own. When taken with insulin or sulfonylureas, the effect multiplies. Even a single glass of tonic water daily can be risky for some.
- Alcohol: Especially on an empty stomach, alcohol blocks the liver from releasing glucose. If you’re on insulin or sulfonylureas, drinking can cause a delayed hypoglycemic episode-sometimes hours after you’ve gone to bed.
What to Do If You’re on Multiple Medications
If you’re taking more than two medications-especially if one of them is for diabetes-here’s what you need to do:- Make a full list: Include every pill, patch, injection, supplement, and herbal product. Don’t leave anything out-not even the fish oil or vitamin D.
- Bring it to every appointment: Your doctor may not ask. But you should show it anyway. Pharmacists can run interaction checks too. Use the pharmacy’s free screening service.
- Monitor your blood sugar more often: When starting or changing any new drug-even an antibiotic-check your glucose before meals and at bedtime for the first week. Look for patterns: Are your numbers dropping after lunch? Spiking after a new painkiller?
- Know the warning signs: Shaking, sweating, confusion, rapid heartbeat? That’s hypoglycemia. Excessive thirst, frequent urination, blurry vision? That’s hyperglycemia. Don’t wait for a meter reading. Act fast.
- Ask about alternatives: If your doctor prescribes a new drug, ask: “Is there a version that won’t interact with my diabetes meds?” Sometimes there’s a different antibiotic, a different pain reliever, or a different diabetes drug that works just as well without the risk.

When to Call for Help
You don’t need to panic every time you start a new medication. But there are times when you need to act immediately:- Your blood sugar drops below 70 mg/dL and doesn’t rise after eating or drinking 15g of fast-acting sugar (like juice or glucose tabs).
- You feel confused, slurred speech, or can’t wake up after a low.
- Your blood sugar stays above 300 mg/dL for more than two days, even with extra insulin.
- You notice sudden swelling in your ankles, shortness of breath, or unexplained weight gain (signs of fluid retention from rosiglitazone or insulin).
If any of these happen, call your doctor or go to urgent care. Don’t wait until your next appointment. A few hours can make the difference between recovery and hospitalization.
The Bottom Line
Managing diabetes isn’t just about counting carbs or checking your meter. It’s about understanding how every drug you take-prescribed, bought over the counter, or even sipped in tonic water-can change how your meds work. The safest approach isn’t taking the most drugs. It’s taking the right ones, together, with full awareness of the risks.GLP-1 RAs and SGLT-2 inhibitors are now the preferred backbone for combination therapy. Older drugs like sulfonylureas and thiazolidinediones carry higher interaction risks. And when in doubt-always check. A five-minute conversation with your pharmacist could prevent a trip to the ER.
Can I take ibuprofen with metformin?
Yes, occasional use of ibuprofen is generally safe with metformin. But long-term or high-dose NSAIDs can reduce kidney function, which increases the risk of metformin buildup. If you’re taking ibuprofen daily for arthritis or back pain, talk to your doctor about switching to a safer pain reliever like acetaminophen or checking your kidney function every 3-6 months.
Do antibiotics affect blood sugar?
Some do, some don’t. Macrolides like clarithromycin and azithromycin can cause hypoglycemia when taken with sulfonylureas or meglitinides. Fluoroquinolones like ciprofloxacin can cause both high and low blood sugar. Always monitor glucose closely during antibiotic treatment, and let your prescriber know you have diabetes. There are often alternative antibiotics with lower interaction risk.
Is it safe to combine insulin with a GLP-1 RA?
Yes, and it’s often recommended. Combining insulin with a GLP-1 receptor agonist like semaglutide or dulaglutide gives better A1C control than insulin alone, with fewer low-blood-sugar episodes and less weight gain. Many patients find this combo easier to manage long-term. Your doctor will adjust your insulin dose downward when starting the GLP-1 RA to prevent hypoglycemia.
Can I drink alcohol if I’m on diabetes medication?
Moderate alcohol (one drink per day for women, two for men) is usually okay if you eat with it. But never drink on an empty stomach, and avoid sugary mixers. Alcohol can cause delayed hypoglycemia, especially with insulin or sulfonylureas. Always check your blood sugar before bed after drinking, and keep fast-acting carbs nearby.
What should I do if I start a new medication and my blood sugar changes?
Track your glucose levels for the next 5-7 days. Note the time of day, meals, and when you took the new drug. If you see a consistent pattern-like lows after lunch or highs after taking a pill-call your doctor or diabetes educator. Don’t adjust your dose on your own. Changes need to be calculated based on your overall pattern, not a single reading.
Staying safe with diabetes meds isn’t about memorizing every interaction. It’s about staying alert, asking questions, and knowing your body’s signals. Your health isn’t just about the pills you take-it’s about how they work together.
Sean McCarthy
December 3, 2025 AT 03:20Don't mix metformin with NSAIDs long term. Kidneys get stressed. Simple as that. Stop ignoring the fine print.
Jaswinder Singh
December 3, 2025 AT 15:59Bro this post is fire. But you missed one thing - fluconazole isn’t the only fungus killer that wrecks your sugar. I took voriconazole last year and my BG dropped to 38 while eating a sandwich. No joke. ER at 2am. Docs didn’t even know. Don’t trust your pharmacist. Trust your meter.
Courtney Co
December 4, 2025 AT 18:01I just started semaglutide and I’m crying because I finally feel like myself again. My husband says I’m too emotional but I haven’t had a hypoglycemic episode in 8 weeks. I used to wake up shaking, drenched in sweat, terrified. Now I sleep. I’m not just managing diabetes. I’m living. Thank you for writing this. I needed to hear someone say it out loud.
James Steele
December 6, 2025 AT 11:00It’s not merely about pharmacokinetic interactions - it’s about the epistemic hegemony of the CYP450 paradigm. The pharmaceutical industrial complex has weaponized enzyme inhibition as a profit vector, while obfuscating the metabolic plasticity of SGLT-2 inhibitors. GLP-1 RAs aren’t just ‘safer’ - they’re ontologically superior. Your insulin-centric model is a relic of the 1980s. The data in The Lancet isn’t suggestive - it’s paradigm-shifting. You’re still thinking in terms of glycemic control. We’re now in the era of metabolic reprogramming.
Louise Girvan
December 7, 2025 AT 18:27St. John’s Wort? Of course it’s dangerous. Big Pharma doesn’t want you to know herbs work. They profit from your dependence. And don’t get me started on the CDC’s silent cover-up of metformin-lactic acidosis deaths. They’ve been burying reports since 2017. Your doctor? He’s on their payroll. Check your blood sugar. Now. I’m not joking.
soorya Raju
December 7, 2025 AT 22:34u think fluconazole is bad? Try ketoconazole shampoo on your scalp every day for 3 months. My sugar went nuts. Doc said ‘it’s not possible’ - then I showed him the bottle. He apologized. Also, tonic water? Nah bro. That’s just sugar water with poison. I switched to seltzer. My A1c dropped 1.4. You’re welcome.
Dennis Jesuyon Balogun
December 8, 2025 AT 10:25This is why community matters. In Nigeria, we call this ‘medicine soup’ - when your body becomes a battlefield of pills. I’ve seen elders die from mixing traditional herbs with metformin because no one explained the science. Knowledge is not just power - it’s survival. If you’re on more than three drugs, sit down with someone who understands pharmacology. Not your cousin who watches YouTube. Someone who reads journals. Your life isn’t a gamble.
Grant Hurley
December 9, 2025 AT 01:30just started taking semaglutide last month and wow. i lost 12 lbs without trying. my sugar’s been stable. i still check like a maniac but it’s way easier. also, i drink one beer after dinner now and don’t freak out. big win. thanks for the tips, this post saved my sanity.
Nnaemeka Kingsley
December 9, 2025 AT 18:32bro if you on insulin and start a new med, check your sugar before bed. i did. missed it once. woke up at 3am with heart racing. thought i was dying. turned out i was low. kept glucose tabs by my bed ever since. simple. free. life saving.
Kshitij Shah
December 11, 2025 AT 02:04Oh wow, so now we’re supposed to stop drinking tonic water because of quinine? Next you’ll tell me to avoid mangoes because they have ‘natural insulin mimics’ and cause hypoglycemia. You know what’s worse than drug interactions? Fear-mongering disguised as medical advice. I’ll take my gin and tonic, thanks.
Bee Floyd
December 12, 2025 AT 22:37Thank you for the detailed breakdown. I’ve been on metformin for 12 years and just learned last month that contrast dye requires a pause. My last CT scan was 2 years ago - I didn’t know. I’m going to print this and take it to my next appointment. Small steps. Big impact.