When you’re told you need chemotherapy, your mind races through the immediate fears: side effects, fatigue, losing your hair. But one question that often gets buried under the noise is: fertility preservation. If you’re someone who might want to have children later, this isn’t a luxury-it’s a critical part of your cancer care plan. The truth? Many people don’t even know these options exist until it’s too late.
Why This Matters More Than You Think
Chemotherapy doesn’t just target cancer cells. It attacks fast-growing cells everywhere-including those in your ovaries and testes. About 80% of common chemo regimens, especially those used for breast cancer, lymphoma, and leukemia, can permanently damage your ability to have biological children. For women, this often means early menopause. For men, it can mean zero sperm production. The damage isn’t always obvious right away. Some people think they’ll just "try later," but the clock doesn’t stop.What You Can Do: The Main Options
There are six proven ways to protect your fertility before chemo starts. Not all apply to everyone, but knowing them gives you power.1. Sperm Banking (For Men)
This is the simplest, most reliable option. Men produce sperm daily, so all it takes is 2-3 days of abstinence, then a sample collected in a private room at a fertility clinic. The sample is frozen using a glycerol-based solution and stored indefinitely. Post-thaw, about 40-60% of sperm remain active. Success rates? If you freeze even one good sample, you can use it years later with IVF or IUI. No stimulation. No surgery. No delay. Most men can complete this in under a week.2. Egg Freezing (Oocyte Cryopreservation)
For women, egg freezing is the most common path. It starts with 10-14 days of daily hormone injections to stimulate your ovaries. You’ll get ultrasounds and blood tests to track growth. Then, under light sedation, eggs are retrieved through a thin needle guided by ultrasound. The eggs are instantly frozen using a method called vitrification, which prevents ice crystals from forming. Survival rates? 90-95%. Each frozen egg has about a 4-6% chance of leading to a live birth. Most women need to freeze 15-20 eggs to have a decent shot at one child. The catch? You need time. And money. But now, many clinics offer "random-start" protocols-meaning you can begin stimulation even if you’re not on your period, cutting the wait down to just 11 days on average.3. Embryo Freezing
This is similar to egg freezing, but the eggs are fertilized with sperm (from a partner or donor) before freezing. Embryos survive freezing better than eggs, and the success rate per transfer is higher: 50-60% for women under 35. The downside? You need sperm. That’s not always possible if you’re single, not in a relationship, or if your partner isn’t ready. But if you have a partner who’s on board, this is the most effective option currently available.4. Ovarian Tissue Freezing
This is the only option for girls who haven’t hit puberty, or for women who can’t wait 10-14 days for hormone stimulation. A small piece of ovarian tissue (about the size of a paperclip) is removed through a quick laparoscopic surgery. It’s frozen in pieces and stored. Later, when you’re cancer-free, the tissue is re-implanted. It can restart hormone production and even allow natural conception. Success rates? Around 65-75% of women regain ovarian function after transplant. Over 200 live births have been reported worldwide. It’s still considered "experimental" by the FDA, but it’s now widely offered at major cancer centers. And here’s the big win: it doesn’t delay chemo.5. Ovarian Suppression with GnRHa
This isn’t a guarantee, but it’s a low-risk backup. You get monthly shots of drugs like goserelin (Zoladex), which temporarily shut down your ovaries during chemo. Studies show it can reduce the risk of early menopause by 15-20%. It’s not as effective as freezing eggs or tissue, but it’s safe, reversible, and doesn’t require surgery or delays. Many women use it alongside egg freezing for extra protection. The side effects? Hot flashes, night sweats, mood swings-like menopause, but temporary. About one in three women stop the shots because they’re too uncomfortable.6. Radiation Shielding (For Pelvic Radiation)
If you’re getting radiation to your pelvis or abdomen, lead shields can block up to 90% of the radiation from reaching your ovaries or testes. This is a simple, non-invasive step that’s often overlooked. Ask your radiation oncologist if it’s possible. It won’t help with chemo damage, but it’s free protection against another threat.What’s the Best Choice?
There’s no single answer. It depends on your age, cancer type, treatment timeline, and personal situation.- If you’re a man: sperm banking is your best-and easiest-move.
- If you’re a woman under 35 with time: egg or embryo freezing gives you the highest odds.
- If you’re a girl or young woman with no time: ovarian tissue freezing is your only option.
- If you’re unsure or can’t freeze: GnRHa shots are a low-risk safety net.
- If you’re getting pelvic radiation: shielding is a must.

Timing Is Everything
You have a narrow window. For most cancers, you need to start fertility steps within days of diagnosis. Acute leukemia patients may have only 48-72 hours before chemo begins. Even for breast cancer, waiting two weeks can mean losing your chance. The average patient misses out because they’re not referred early enough. That’s why experts say: as soon as you hear "cancer," ask for a fertility consult. Don’t wait. Don’t assume your oncologist will bring it up. Many don’t. In fact, only 37% of eligible patients complete any form of preservation-mostly because they weren’t offered the option in time.Cost, Insurance, and Access
This is where things get messy. Egg freezing can cost $10,000-$15,000 per cycle. Sperm banking? Around $500-$1,000. Ovarian tissue freezing? $8,000-$12,000. Insurance coverage varies wildly. In 24 U.S. states, insurers are required to cover fertility preservation for cancer patients. In Australia, Medicare doesn’t cover it unless you’re in a clinical trial. Medicaid covers it in only 12 states. Rural patients often travel over 170 miles to reach a fertility center. If you’re struggling to pay, ask your hospital’s social worker. Many centers offer payment plans, discounts, or grants through nonprofit groups like the Live Strong Foundation or the Oncofertility Consortium.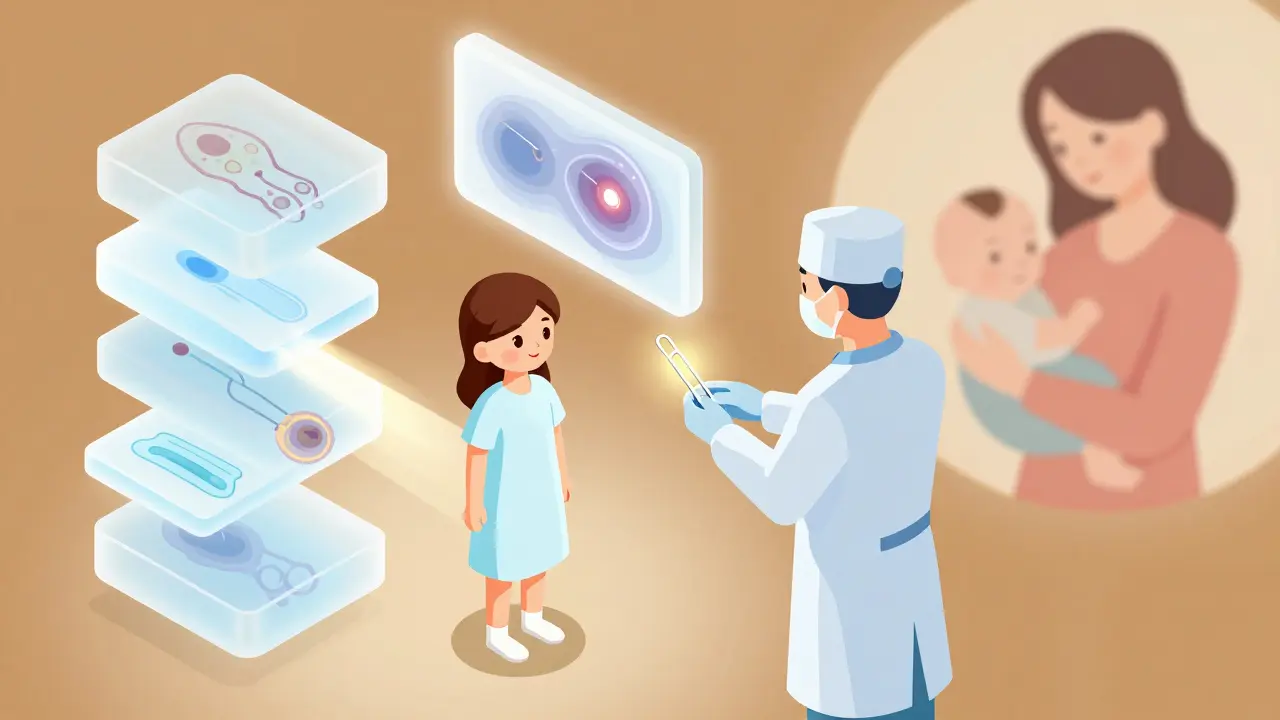
What About the Future?
Science is moving fast. In 2023, the FDA approved a new closed-system vitrification device that cuts contamination risk by 92%. Researchers are now testing "artificial ovaries"-lab-grown tissue that could replace transplanted tissue entirely. One study in primates showed 68% follicle survival. That’s not human yet, but it’s coming. The goal? A future where no cancer patient has to choose between life and family.Real Stories, Real Pain
A 29-year-old woman in Sydney, diagnosed with breast cancer, found out too late that egg freezing took too long. She started chemo, lost her period, and now, three years later, she says: "I never thought I’d want kids this badly. I wish someone had told me sooner." On Reddit, a man with Hodgkin’s lymphoma shared: "I froze my sperm in 48 hours. It was the only thing I felt I could control. Now I have a daughter thanks to that tiny vial." These aren’t rare cases. They’re the norm.What to Do Right Now
If you or someone you love is facing chemotherapy:- Ask your oncologist: "Can you refer me to a fertility specialist today?"
- If they say no, ask for the name of the nearest oncofertility clinic. Google "oncofertility program near me."
- For men: Go to a sperm bank immediately. No waiting.
- For women: If you have time, start egg or embryo freezing. If you don’t, ask about ovarian tissue freezing.
- Ask about GnRHa shots-even if you’re freezing, they add protection.
- Ask about radiation shielding if you’re getting radiation.
- Don’t assume it’s too expensive. Ask about financial help.
Chemotherapy saves lives. But it doesn’t have to steal your future. Fertility preservation isn’t about being selfish. It’s about giving yourself a choice after survival.
Can I still have kids after chemotherapy if I didn’t preserve my fertility?
Some people do. About 20-30% of women regain natural fertility after chemo, especially if they’re younger and didn’t receive high-dose alkylating agents. Men may still produce sperm, though often at low levels. But it’s unpredictable. If you didn’t preserve, don’t assume you’re out of options-consult a reproductive specialist. IVF with donor eggs or sperm, surrogacy, or adoption are still paths to parenthood.
How long can frozen eggs, sperm, or tissue be stored?
There’s no known expiration date. Frozen sperm has been used successfully after 30+ years. Frozen embryos have resulted in healthy births after 25 years. Ovarian tissue has been thawed and transplanted after 10 years with success. Storage is indefinite as long as the facility maintains proper cryogenic conditions.
Does fertility preservation increase cancer risk?
No. Studies show no link between hormone stimulation for egg freezing and cancer recurrence, even in hormone-sensitive cancers like breast cancer. The short-term estrogen rise from stimulation doesn’t trigger cancer growth. Major cancer centers now routinely offer this to breast cancer patients.
Can I do fertility preservation if I’m not married or don’t have a partner?
Yes. Egg freezing doesn’t require a partner. You can use donor sperm later if you choose. Embryo freezing requires sperm, so you’d need a donor. Many single women choose egg freezing for this reason. Clinics are used to working with single patients-it’s common.
Is fertility preservation covered by Medicare in Australia?
Medicare doesn’t cover the cost of egg freezing, sperm banking, or ovarian tissue freezing unless you’re part of an approved clinical trial. Some private health insurers offer partial coverage under extras policies, but you’ll likely pay out-of-pocket. Check with your insurer and ask your hospital’s financial counselor about grants or payment plans.
Terry Free
December 24, 2025 AT 15:26Let me get this straight - you’re telling me we’ve got people walking around with cancer diagnoses who don’t know they can freeze their sperm in 48 hours? Bro. That’s not ignorance. That’s negligence. If your oncologist doesn’t bring this up, fire them. Sperm banking is cheaper than a Starbucks subscription. You’re not saving your future - you’re saving your damn dignity.
And don’t get me started on the ‘I’ll just adopt’ crowd. Adoption is beautiful. But it’s not a substitute for biological legacy. Stop romanticizing it like it’s a moral upgrade. You want kids? Preserve your genes. End of story.
Sophie Stallkind
December 25, 2025 AT 11:31It is with profound respect for the medical and ethical complexities involved that I offer this observation: the integration of oncofertility protocols into standard oncology care represents a paradigmatic shift in patient-centered medicine. The absence of routine referrals for fertility preservation constitutes a systemic failure in patient advocacy, particularly for populations with limited health literacy or socioeconomic resources. Institutions must implement mandatory multidisciplinary consultations at the time of diagnosis, ensuring equitable access to reproductive autonomy as a non-negotiable component of comprehensive cancer care.
Mussin Machhour
December 25, 2025 AT 12:57Y’all need to hear this: if you’re facing chemo, your fertility isn’t a side note - it’s your future. I’ve seen guys cry because they waited too long. I’ve seen women regret not asking. Don’t be one of them. Go to the clinic TODAY. Even if you’re scared. Even if you’re broke. There are grants. There are payment plans. There are people who want to help.
You’re not just fighting cancer. You’re fighting for the chance to hold your kid someday. That’s worth every second, every dollar, every awkward conversation. You got this.
Katherine Blumhardt
December 25, 2025 AT 21:01ok so i just found out my cousin is doing chemo and she didnt know about freezing eggs and now shes like oh nooo but wait i think i heard something about like ovaries being cut out and frozen??? is that real?? or is that just a tiktok thing?? also i think my aunt said something about like a shot that stops your period?? is that the same thing?? please help i dont wanna mess this up for her 😭
Linda B.
December 26, 2025 AT 12:06Let’s not pretend this is about choice. It’s about control. Who benefits from pushing fertility preservation? Pharma. Clinics. The fertility-industrial complex. They make billions off frozen eggs and IVF cycles. Meanwhile, the real issue - why cancer treatments are so brutally destructive to the human body - gets ignored. Why aren’t we funding research into targeted therapies that don’t wreck ovaries and testes? Why are we turning patients into gamete banks instead of fixing the root problem?
And yes, I know they say it’s safe. But have you read the long-term studies on hormone stimulation and estrogen-sensitive tumors? No? Then don’t pretend you’re being proactive. You’re being manipulated.
Winni Victor
December 28, 2025 AT 12:05Oh wow, so now we’re supposed to be grateful that we can freeze our reproductive organs like leftover lasagna? ‘Oh honey, I saved your sperm in a vial labeled ‘Doomed Hope #3’ - it’s in the cryo freezer next to the frozen peas.’
Look, I get it. You want kids. But let’s be real - if you’re going through chemo, your life is already on fire. Do you really think your future kid is gonna be like, ‘Mom, I’m so glad you sacrificed your mental health and $15K to give me a chance at life… while you were still puking in a hospital bed’?
Adoption is cheaper. Less traumatic. And your kid won’t have to Google ‘Why did my mom cry every time she saw a stroller?’
Also, sperm banking? That’s just a guy wanking into a cup while his body is being nuked from the inside. How romantic.
Zabihullah Saleh
December 28, 2025 AT 13:44There’s something quietly sacred about preserving life while you’re fighting death. It’s not about biology - it’s about continuity. The sperm, the egg, the tissue - they’re not just cells. They’re echoes of who you were before the diagnosis. They’re hope made physical.
I’ve sat with people who lost their fertility and spent years mourning a future they never got to choose. It’s not a luxury. It’s a quiet act of defiance against chaos. The body breaks. But the will to create? That’s harder to kill.
Bailey Adkison
December 29, 2025 AT 18:51Claiming that sperm banking is 'simple' is misleading. It requires transportation to a clinic, scheduling, abstinence protocols, and psychological readiness. Many men are culturally conditioned to view semen donation as emasculating. This isn't a medical issue - it's a social one. And the assumption that women have 'time' for egg freezing ignores the reality of aggressive cancers. The article reads like a marketing brochure for fertility clinics. Where are the real barriers? Where are the stories of people who couldn't afford it? Where are the data on long-term outcomes? You're not informing. You're selling.
Carlos Narvaez
December 30, 2025 AT 19:24Freeze your eggs. Freeze your sperm. Freeze your hopes. The system doesn’t care if you have kids. It cares if you survive. And even then, you’ll be lucky if you’re alive to see them graduate college.
Save your money. Save your energy. Save your dignity.
Adoption is real. Biology is a gamble.
Harbans Singh
January 1, 2026 AT 09:51This is beautiful. In India, we don’t talk about this. My cousin had chemo and thought she’d never be a mom. She found out about ovarian tissue freezing through a nonprofit. Now she has a daughter. It’s not just science - it’s hope.
But here’s the thing - we need this info in more languages. In villages, people still think chemo = death. No one tells them about eggs or sperm. I’m sharing this with my community. Thank you for writing this. You saved someone’s future.
Oluwatosin Ayodele
January 1, 2026 AT 13:40You people are wasting time talking about freezing eggs and sperm. The real issue is that cancer is caused by toxins in the food, water, and vaccines. The pharmaceutical companies don’t want you to know that fertility preservation is just a distraction. They profit more from chemo than from IVF. They don’t want you to find out that your body can heal naturally if you stop eating processed sugar and take turmeric.
Also, why do you think they only offer this to people in the US and Australia? Because they’re testing population control. The real fertility crisis is caused by glyphosate and 5G. Ask yourself - who benefits?