Many people take generic drugs without a second thought. But for others, the very word generic triggers doubt. Is it really the same? Will it work? Could it hurt me? These aren’t just random worries-they’re deeply rooted perceptions that shape whether someone fills a prescription, sticks with it, or switches back to the brand name, even when it costs three times as much.
Why Do People Think Generics Are Less Safe?
The science says otherwise. The FDA requires generic drugs to match brand-name drugs in strength, purity, and how the body absorbs them. They must be bioequivalent-meaning they work in the body within a tight 80% to 125% range of the original. That’s not a guess. It’s a strict, tested standard. Yet, nearly one in five patients still believe generics are less safe. Why? It’s not about the drug. It’s about the label. The word "generic" carries baggage. People associate it with "cheap," "inferior," or "second-rate." That’s not how the FDA sees it. But for many, cost equals quality. If a brand-name pill costs $10 and the generic costs $3, the brain automatically assumes the cheaper one must be cut corners. This bias isn’t unique to medicine. People think a $200 watch is better than a $20 one-even if they’re made in the same factory. Add to that the fact that generics look different. Same active ingredient, but a different shape, color, or imprint. When someone switches from their familiar blue oval pill to a white round one, it feels like a different medicine. That’s not a trick of the mind-it’s a real psychological shift. One patient told a pharmacist, "I know it’s the same drug, but this one doesn’t feel right." That feeling matters more than data.Who’s Most Likely to Worry?
Not everyone sees generics the same way. Risk perception isn’t random-it lines up with who you are. Older adults, especially those over 60, are more likely to fear side effects. They’ve been on medications longer. They’ve seen what happens when things go wrong. A change in pill appearance feels like a gamble they didn’t sign up for. People with lower education levels are nearly twice as likely to think generics are dangerous. They’re less likely to understand terms like "bioequivalence" or "active ingredient." They don’t know the FDA inspects generic factories the same way it inspects brand-name ones. They hear rumors: "My cousin’s friend took a generic and got sick." Racial and ethnic minorities, particularly Black and Hispanic patients, are 1.8 times more likely to express safety concerns than white patients. This isn’t about distrust in science-it’s about distrust in systems. Historical mistreatment, language barriers, and unequal access to clear information all play a role. Rural patients often believe generics are weaker and need higher doses. They think, "If it’s cheaper, it must be less potent." Urban patients, meanwhile, worry more about where the drug was made-"Is it coming from a dirty factory?" Even employment status matters. Unemployed or retired people are more open to generics. They’ve seen the cost difference up close. Employed people, who often have insurance that covers brand names, are more likely to stick with what they know-even if it’s more expensive.What Happens When You Switch?
Stories matter more than statistics. There are thousands of posts on Reddit, PatientsLikeMe, and forums where people say: "I switched to generic sertraline and had panic attacks." Or, "My blood pressure shot up after my doctor switched me to the generic version." These aren’t rare. They’re real experiences. The FDA did issue a safety notice in 2012 about certain generic versions of bupropion XL-some patients reported reduced effectiveness. That case, though limited, became a poster child for skepticism. Even though the FDA later confirmed most generics were fine, the damage stuck. Here’s the twist: most people who switch to generics report no difference at all. A 2021 survey found 68% saw no change in side effects or effectiveness. But the 32% who did notice something? They’re the ones who tell their friends, their family, their support groups. One bad experience can outweigh ten good ones. And here’s the cruel irony: patients who report problems after switching often go back to the brand. They don’t blame the system. They don’t blame their doctor. They blame the generic. They think, "This one just doesn’t work like the other one." But the truth? Sometimes, the brand version itself changed. Sometimes, the patient’s condition changed. Sometimes, the placebo effect wore off. But the mind doesn’t look for those explanations. It looks for the easiest one: the generic is different.
How Doctors and Pharmacists Can Help
The biggest factor in whether someone accepts a generic? What their doctor says. A 2011 study found patients were 3.2 times more likely to take a generic if their doctor explained why it was safe. Not just: "It’s cheaper." But: "This generic has the same active ingredient, same dosage, and was tested to work exactly like the brand. The FDA checks every batch. It’s not a different drug-it’s the same medicine, just without the marketing cost." But too often, that conversation doesn’t happen. Doctors are rushed. Pharmacists have 47 seconds on average to talk to a patient about a generic substitution. That’s not enough time to explain bioequivalence or reassure someone who’s scared. The best results come from clear, simple, repeated messaging. A 2017 study showed that low-health-literacy patients who got tailored education-using pictures, simple words, and real-life examples-reduced their safety concerns by 42%. One tool that worked? Showing side-by-side photos of brand and generic pills with labels saying: "Same medicine. Different look. Same effect." Pharmacists who take the extra minute to say, "I know you’re used to the blue pill. This one’s white, but it’s the same drug. I’ve filled this for hundreds of people. No one’s had a problem," makes a difference. That personal touch builds trust.Why This Matters Beyond the Prescription
This isn’t just about how someone feels about a pill. It’s about money, health, and fairness. Generics make up 90% of all prescriptions in the U.S. But they account for only 23% of drug spending. That’s $370 billion saved every year. If everyone took generics when they could, the system could save another $185 billion over the next decade. But right now, about $8 billion a year is wasted because people insist on brand names-even when they don’t need them. Insurance companies push generics because they’re cheaper. But if patients refuse them out of fear, the system pays more. And patients pay more too-through higher premiums, copays, and out-of-pocket costs. The problem isn’t the drugs. It’s the story. The story that generics are risky. The story that cheaper means worse. The story that if it doesn’t look the same, it’s not the same. The FDA, AARP, and health advocates have made good materials. AARP’s guide on generics scored 4.5 out of 5 for clarity. The FDA’s own page? Only 3.2. That’s a gap. And it’s a gap that costs lives.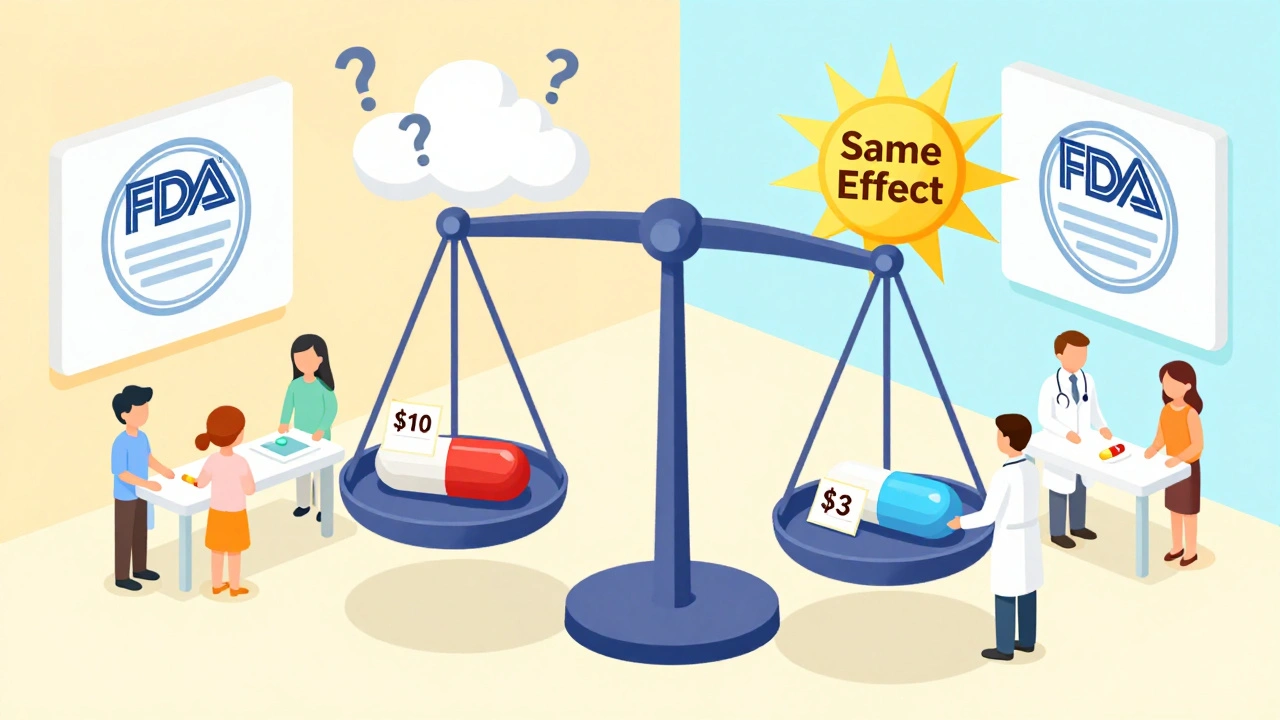
What Can You Do?
If you’re on a generic drug and you’re worried:- Ask your pharmacist: "Is this the same as the brand?" They can show you the FDA’s approval data.
- Ask your doctor: "Why did you choose this generic?" Don’t be afraid to ask for the science.
- Track your symptoms. If you feel worse after switching, write it down. But don’t assume it’s the drug. Talk to your provider before switching back.
- Check if your insurance offers $0 copays for generics. Many do. That removes the cost barrier and makes the switch easier.
- Don’t assume patients understand. Use plain language. Say: "This is the same medicine. Just a different name and look."
- Use visual aids. Show the pills side by side.
- Don’t wait until the pharmacy. Talk about generics at the time of prescribing. That’s when patients are most open.
What’s Next?
New tools are emerging. Machine learning can now predict which patients are most likely to resist generics-with 87% accuracy. That means clinics can target education where it’s needed most. The FDA is running multilingual campaigns. They’re putting info in Spanish, Mandarin, and Vietnamese. Early results show a 15% drop in safety fears among Spanish-speaking patients. But the real fix? It’s not a campaign. It’s a conversation. It’s a doctor taking five extra minutes. A pharmacist offering a handout. A nurse saying, "I’ve seen this work for thousands. I’d take it myself." Because at the end of the day, safety isn’t just about chemistry. It’s about trust.Are generic drugs really as safe as brand-name drugs?
Yes. The FDA requires generic drugs to meet the same strict standards as brand-name drugs for strength, quality, purity, and how the body absorbs them. Every generic must prove it works the same way in the body. The only differences are in color, shape, or inactive ingredients-none of which affect safety or effectiveness.
Why do some people feel worse after switching to a generic?
Sometimes, the change in pill appearance triggers psychological effects. Other times, it’s a coincidence-their condition changed, or they stopped taking it consistently. Rarely, a specific generic version may have had a manufacturing issue (like with some bupropion XL versions in 2012). But these cases are uncommon. Most people notice no difference. If you feel worse, talk to your doctor before switching back.
Can I ask my doctor to keep me on the brand-name drug?
Yes. If you have a valid reason-like a previous bad reaction to a specific generic, or a condition where even small changes matter (like epilepsy or thyroid meds)-your doctor can write "Do Not Substitute" on the prescription. But if there’s no medical reason, generics are just as safe and save you money.
Do generic drugs come from lower-quality factories?
No. The FDA inspects all drug factories-brand and generic-using the same standards. Many generic drugs are made in the same facilities as brand-name versions. The FDA has found no evidence that generic manufacturing is less safe. In fact, over 50% of generic drugs in the U.S. are made in U.S.-based facilities.
Why do generics look different if they’re the same?
Brand-name companies hold patents on pill shapes and colors. Once the patent expires, generic makers can’t copy the exact look. So they change the color, size, or imprint. That’s why your generic pill might be white instead of blue-but it still contains the exact same active ingredient and works the same way.
Are there any drugs where generics aren’t recommended?
For most drugs, generics are equally effective. But for a few narrow-therapeutic-index drugs-like warfarin, levothyroxine, or certain seizure meds-small changes in blood levels can matter. In these cases, doctors may recommend sticking with one brand or generic version to avoid fluctuations. But even here, switching between approved generics is usually safe if monitored properly.
How can I tell if my generic is FDA-approved?
Look for the drug’s name on the label. All FDA-approved generics must list the active ingredient and manufacturer. You can also check the FDA’s online database, "Drugs@FDA," or ask your pharmacist to show you the approval information. If it’s sold in a U.S. pharmacy, it’s been reviewed and approved.
Donna Hammond
December 14, 2025 AT 10:09I used to be terrified of generics after my mom had a bad reaction to one-turned out it was just her thyroid meds switching brands and her body needed time to adjust. I didn’t know that until I sat down with her pharmacist and he showed me the FDA approval docs side by side. Same active ingredient. Same absorption rate. Just a different color. That visual made all the difference. Now I take generics without a second thought-and I’ve convinced three of my friends to do the same.
Richard Ayres
December 16, 2025 AT 00:33The data is clear, the regulatory framework is robust, and the cost-benefit analysis is overwhelmingly favorable. Yet public perception remains stubbornly misaligned with evidence. This is not a failure of science communication alone, but of systemic trust deficits rooted in historical inequities and fragmented healthcare delivery. Addressing this requires not only clearer messaging but structural reform in patient-provider interaction time and access to consistent, culturally competent education.
Scott Butler
December 16, 2025 AT 11:23Why are we even having this conversation? If you’re too cheap to pay for a real drug, maybe you shouldn’t be taking medicine at all. The FDA doesn’t care about your feelings. If you want the real thing, pay for it. Stop crying because your pill looks different. This country is falling apart because people think they deserve something for nothing.
Emma Sbarge
December 17, 2025 AT 01:58My cousin’s husband took a generic for his blood pressure and ended up in the ER. They said it was a coincidence, but I’ve seen enough. I don’t care what the FDA says-my family’s health isn’t a lab experiment. If it looks different, smells different, feels different-it’s different. And I’m not risking my life for a $3 savings.
Constantine Vigderman
December 17, 2025 AT 22:55Guys, I switched my anxiety med to generic and I was FREAKING OUT at first-like, full panic mode. But I tracked my sleep, my mood, my heart rate for two weeks. No difference. Zero. And I saved $120 a month. I even made a little chart and showed it to my mom. She’s still skeptical, but she’s watching now. You guys, it’s the same damn pill. Just cheaper. Trust the science, not the color.
Webster Bull
December 19, 2025 AT 09:23Same pill. Different wrapper. That’s it.
Bruno Janssen
December 20, 2025 AT 14:20I don’t even know why I’m reading this. I just took my generic and stared at it for ten minutes. Wondering if it’s going to kill me. I know it’s dumb. I know it’s irrational. But I can’t shake it. I just… feel it. And no amount of data changes that feeling.
Karen Mccullouch
December 21, 2025 AT 14:36My pharmacist gave me a handout with pictures of my brand vs. generic. Same active ingredient. Same FDA stamp. I cried. Not because I was happy-because I realized I’d been scared for years over a color change. I’m not stupid. I just never had someone take the time to show me. Now I tell everyone. If you’re scared, ask. They’ll show you. It’s not magic. It’s medicine.