Every year, thousands of patients in Australia and around the world are harmed by simple mistakes in pharmacies. A pill gets swapped. A dose is miscalculated. A drug interaction is missed. These aren’t rare accidents-they’re preventable errors that happen because human beings are doing complex, high-pressure work under time pressure. The good news? Pharmacy workflow and error prevention systems are changing that. They’re not magic. They’re smart tools built by pharmacists, for pharmacists, to catch mistakes before they reach the patient.
How Medication Errors Happen in Pharmacies
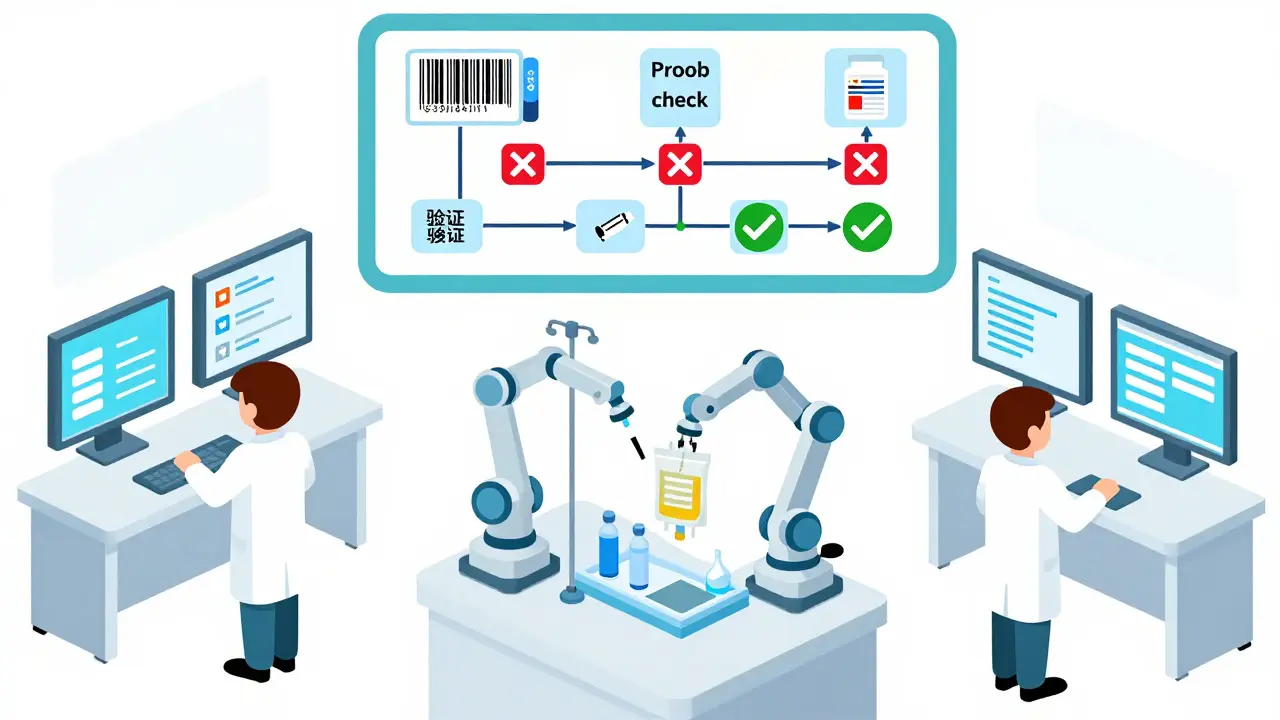
It’s easy to assume that pharmacists are just counting pills. But the reality is far more complex. A single prescription can involve checking the patient’s full medication history, verifying allergies, confirming dosage against age and kidney function, matching the drug to the correct formulation, ensuring it’s not expired, and labeling it clearly-all while juggling ten other requests. One wrong step, one distracted moment, and a patient gets the wrong medicine. In 2024, a study from the Australian Institute of Health and Welfare found that over 20% of dispensing errors in community pharmacies involved incorrect dosage or drug selection. In hospitals, where IV medications are prepared manually, the risk is even higher. A single error in an IV bag can lead to cardiac arrest, organ failure, or death. These aren’t hypotheticals. They’re documented cases. The root cause? Human fatigue, interruptions, poor labeling, and lack of real-time access to patient data. No pharmacist is perfect. But systems can be.What Pharmacy Workflow Systems Actually Do
Pharmacy workflow systems aren’t just fancy robots. They’re integrated networks of hardware and software designed to guide every step of the medication process-from when a prescription arrives to when the patient walks out the door. At the core, these systems do four things:- Automatically verify the right patient, right drug, right dose, right route, right time
- Scan barcodes on every pill bottle, vial, and IV bag to confirm matches
- Check for drug interactions, allergies, and duplicate therapies in real time
- Track inventory and alert staff before medications expire or run low
Key Technologies Behind the Systems
These aren’t sci-fi fantasies. They’re real tools used in hospitals and pharmacies across Sydney and beyond.- Barcode Scanning: Every medication container has a unique barcode. Scanning it at each step confirms it’s the right item. If you scan the wrong one, the system stops you.
- Robotics for Compounding: Devices like BD Pyxis™ and Omnicell’s automated dispensing units handle sterile IV prep. They’re used in 80% of major Australian hospitals.
- Electronic Health Record (EHR) Integration: Systems use HL7 protocols to talk directly to hospital records. No more manual data entry. No more lost charts.
- Inventory Management: The system tracks expiry dates. If a vial of insulin expires in three days, it pops up as a priority item to use-or remove.
- Workflow Automation: Tasks are assigned automatically. One tech checks the order, another prepares the dose, a third verifies it. Each step is logged. No one can skip ahead.

Top Systems Used in Australia and Beyond
Not all systems are the same. Some are built for big hospitals. Others fit in small community pharmacies.- BD Pyxis™: Used in over 60 Australian hospitals. Focuses on automated dispensing and IV compounding. Integrates with Epic and Cerner EHRs.
- Wolters Kluwer’s Simplifi+ IV: Designed specifically for IV compounding centers. Tracks compliance with USP <797> and <800> standards for sterile preparation.
- Cflow: Cloud-based system popular in community pharmacies. Offers templates for daily workflows, refill reminders, and patient follow-ups.
- KanBo: A visual workflow tool used by pharmacy leads to track prescription backlogs, assign tasks, and avoid double bookings.
How Much Do These Systems Cost?
Let’s be honest-these aren’t cheap. A full hospital-grade system can cost between $80,000 and $250,000 per year, depending on features and integration needs. Smaller community pharmacies might spend $15,000-$40,000 for a streamlined version. But the cost of not using them? Much higher. A single medication error can lead to a lawsuit, regulatory fine, or loss of license. In 2023, the Australian Health Practitioner Regulation Agency (AHPRA) reported 120 formal complaints against pharmacies for dispensing errors-up 37% from 2020. The average cost of a resolved error claim? Over $150,000. Plus, there’s the hidden cost of staff burnout. Pharmacists using manual systems report working 12-hour days just to keep up. Those using automated systems say they leave on time-and feel safer doing their jobs.Why Technology Alone Isn’t Enough
Installing a robot doesn’t fix a broken process. Too many pharmacies buy a system, plug it in, and expect miracles. They don’t train staff. They don’t change workflows. And then they wonder why errors keep happening. The American Society of Health-System Pharmacists (ASHP) says it plainly: “Technology must be matched with process redesign.” That means:- Training every technician and pharmacist on how the system works-not just how to click buttons
- Redesigning the physical layout of the pharmacy to match the new workflow
- Creating clear roles: Who scans? Who verifies? Who signs off?
- Testing the system with real prescriptions before going live
Real Results: Numbers That Matter
Don’t take my word for it. Here’s what actual data shows:- Pharmacies using barcode verification reduce dispensing errors by up to 85%
- Hospitals with automated IV compounding cut preparation errors by 92%
- Systems with real-time EHR integration detect 14 times more potential drug interactions than manual checks
- Inventory tracking reduces expired medication waste by up to 40%
What’s Next? AI and Predictive Systems
The next wave isn’t just automation-it’s anticipation. New systems are starting to use AI to predict problems before they happen:- Alerting pharmacists when a patient is likely to miss a dose based on refill history
- Forecasting which medications will run out based on seasonal trends
- Flagging unusual prescribing patterns that might indicate fraud or misuse
Final Thought: Safety Is a System, Not a Person
We used to believe that if we just trained pharmacists better, errors would disappear. But the truth is, humans make mistakes. That’s not a failure-it’s biology. The goal isn’t to find the perfect pharmacist. It’s to build the perfect system. A system that checks twice. A system that reminds. A system that won’t let you skip a step. A system that gives you time to think, not just to rush. Pharmacy workflow and error prevention systems aren’t about replacing people. They’re about protecting them-from burnout, from blame, and from the unthinkable consequence of a single wrong pill. If your pharmacy hasn’t looked at these systems yet, it’s not too late. It’s overdue.How do pharmacy workflow systems reduce medication errors?
They use automated checks like barcode scanning, real-time drug interaction alerts, and electronic verification of patient history to catch mistakes before they happen. For example, if a pharmacist tries to dispense the wrong dose, the system blocks the action and flags the error. Studies show these systems reduce dispensing errors by up to 85%.
Are pharmacy workflow systems only for hospitals?
No. While hospitals use advanced systems for IV compounding, community pharmacies benefit too. Smaller platforms like Cflow and KanBo help with prescription tracking, refill management, inventory alerts, and patient communication-all of which reduce errors in daily operations.
What’s the biggest challenge when implementing these systems?
The biggest challenge isn’t the technology-it’s changing how people work. Staff often resist new systems because they’re used to old routines. Successful implementations require months of training, clear role assignments, and ongoing feedback. Rushing the process leads to errors and frustration.
Do these systems comply with Australian regulations?
Yes. Reputable systems are built to meet Australian standards like TGA guidelines, ASHP best practices, and international standards such as USP <797> for sterile compounding. They also include audit trails and encryption to comply with privacy laws like the Privacy Act 1988 and HIPAA-equivalent protocols.
How long does it take to see results after installing a system?
Most pharmacies see immediate improvements in workflow speed and inventory accuracy. But for error reduction to become consistent, it typically takes 3 to 6 months. This includes training staff, adjusting workflows, and ironing out glitches. The best results come from treating implementation as a process-not a one-time upgrade.
Can these systems prevent all medication errors?
No system is foolproof. But they reduce the most common and dangerous errors-wrong drug, wrong dose, wrong patient-by over 80%. They don’t replace clinical judgment. They support it. The best outcomes happen when technology and pharmacist expertise work together.
For pharmacies still relying on paper logs and manual checks, the gap between safety and risk is growing. The tools to close it exist. The question isn’t whether you can afford to implement them-it’s whether you can afford not to.
Poppy Newman
January 7, 2026 AT 09:10Mina Murray
January 8, 2026 AT 01:51Alex Danner
January 9, 2026 AT 19:52Emma Addison Thomas
January 11, 2026 AT 14:11Christine Joy Chicano
January 11, 2026 AT 21:26Adam Gainski
January 12, 2026 AT 07:41Anastasia Novak
January 13, 2026 AT 13:09Jonathan Larson
January 15, 2026 AT 12:45Katrina Morris
January 17, 2026 AT 08:53Andrew N
January 17, 2026 AT 22:57LALITA KUDIYA
January 19, 2026 AT 07:49Vince Nairn
January 19, 2026 AT 15:25Ayodeji Williams
January 20, 2026 AT 16:01