Rhabdomyolysis Risk Checker
Check Your Medications
Results
Important Safety Note
While this tool identifies potential drug interactions, it does not replace professional medical advice. Always consult your doctor or pharmacist before making changes to your medications.
Most people think of muscle pain after a hard workout. But what if your muscles start hurting for no reason-especially if you’ve recently started a new pill or changed your dose? That could be a red flag for rhabdomyolysis, a serious condition where muscle tissue breaks down and floods your bloodstream with toxic proteins. It’s not rare. And it’s often caused by common drug combinations you might not even think twice about.
What Exactly Is Rhabdomyolysis?
Rhabdomyolysis happens when muscle cells get damaged and leak their contents into your blood. The worst offender? Myoglobin, a protein that turns urine dark red or cola-colored. Your kidneys can’t handle this flood. They clog up. And that’s when things get dangerous. Up to half of people with severe rhabdomyolysis develop acute kidney injury. Some need dialysis. About 5 to 15% die if it’s not caught fast enough.The classic signs-muscle pain, weakness, and dark urine-only show up in about half the cases. Many people just feel tired, nauseous, or have abdominal pain. Some even run a fever. By the time they go to the ER, it’s often too late. That’s why it’s called a silent emergency.
Statins Are the Main Culprit-But Not Alone
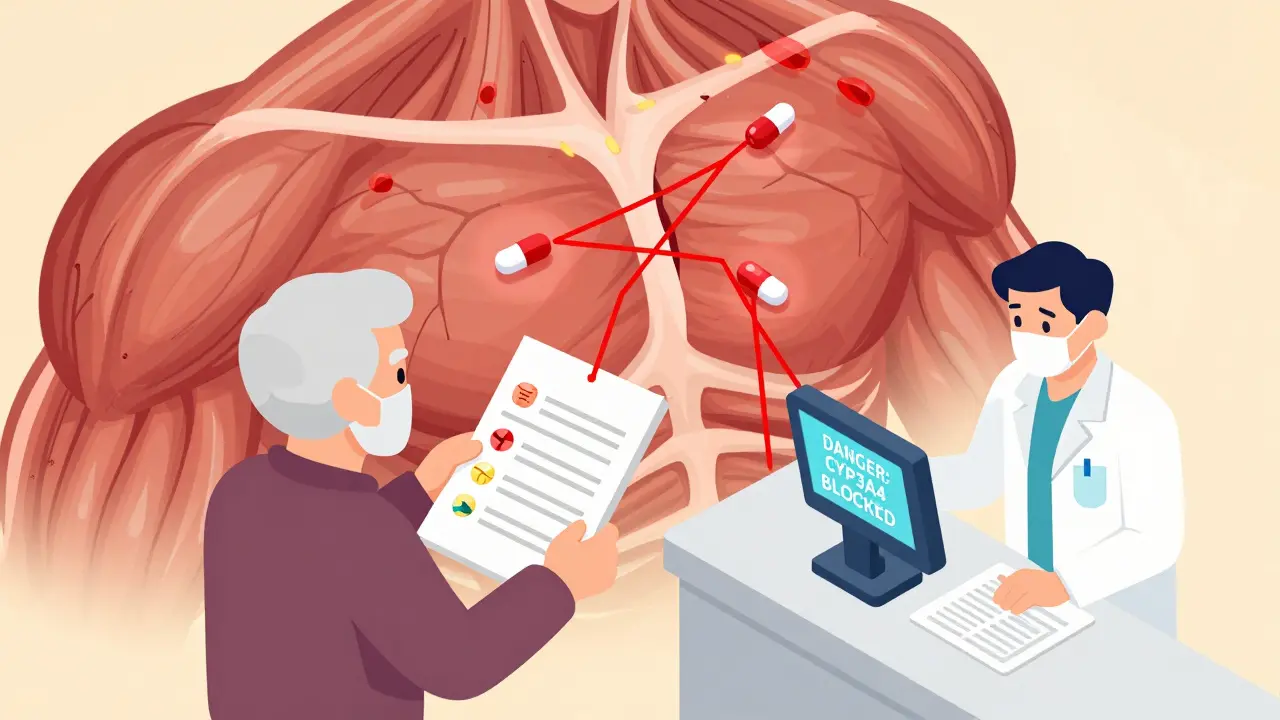
Statins like atorvastatin (Lipitor) and simvastatin (Zocor) cause about 60% of all drug-induced rhabdomyolysis cases. That’s not because they’re unsafe on their own. It’s because they’re so widely used. Over 300 million people worldwide take them. But when you mix them with other drugs, the risk skyrockets.For example, combining simvastatin with the antibiotic erythromycin increases rhabdomyolysis risk by nearly 19 times. Why? Both drugs are broken down by the same liver enzyme-CYP3A4. When one blocks it, the other builds up to toxic levels. It’s like pouring gasoline on a fire you didn’t know was lit.
Even worse? Gemfibrozil (a cholesterol drug) with simvastatin. This combo raises risk by 15 to 20 times. It’s not just the drugs themselves-it’s how they interact. And doctors don’t always catch it.
Other Dangerous Drug Combos You Might Not Know About
It’s not just statins. Other common prescriptions can trigger muscle breakdown too:- Colchicine + clarithromycin: Used for gout and infections. Together, they cause rhabdomyolysis in nearly 9% of cases. The European Medicines Agency issued a strong warning in 2021 after reviewing over 1,200 cases.
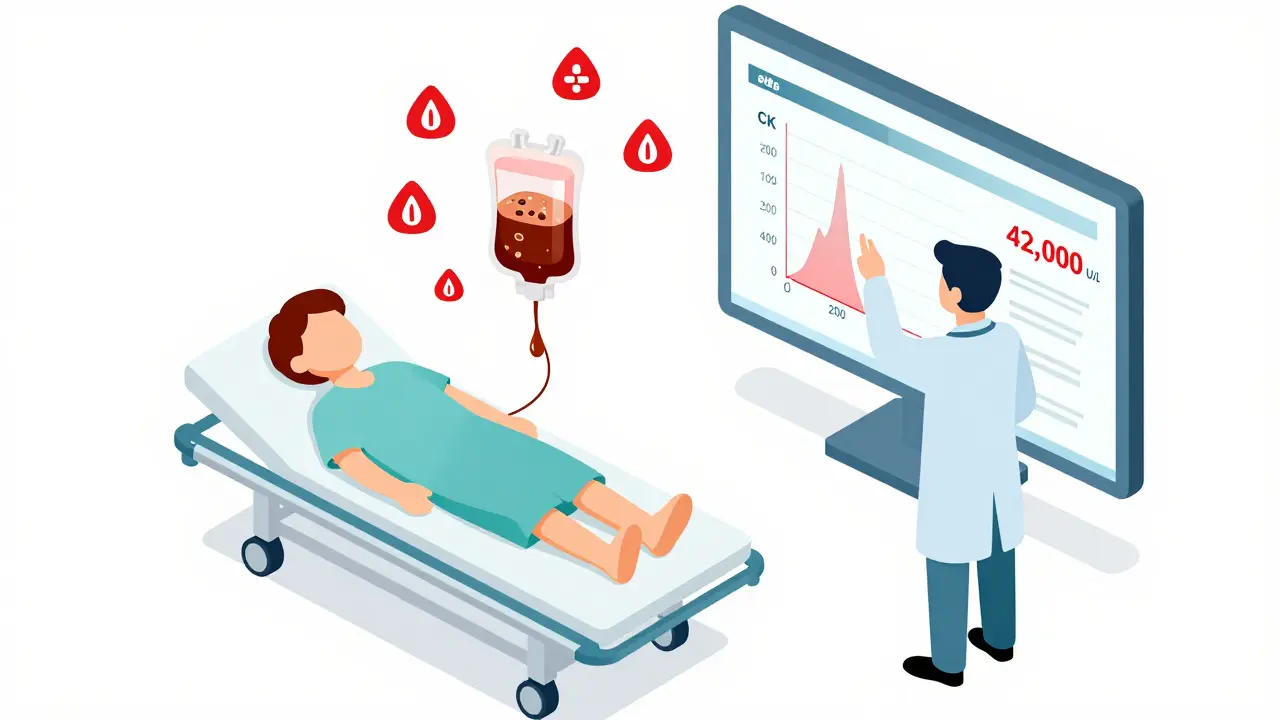
- Erlotinib (cancer drug) + simvastatin: A lung cancer patient taking both saw CK levels hit 42,000 U/L in under 72 hours. Normal is under 200. That’s over 200 times higher.
- Propofol (anesthesia) in ICU patients: Rare, but deadly. When rhabdomyolysis develops, mortality hits 68%. It shuts down energy production in muscle cells.
- Zidovudine (HIV drug): Up to 12% of patients on this drug show CK levels over 10 times normal. It damages mitochondria-the energy factories in your cells.
- Leflunomide (for rheumatoid arthritis): Extremely rare, but CK levels can explode past 50,000 U/L. Plasma exchange is often needed because the drug sticks around for weeks.
These aren’t edge cases. They’re documented in medical journals, FDA reports, and patient forums. One Reddit user wrote: "My oncologist didn’t warn me about the simvastatin-erlotinib interaction-CK peaked at 42,000 and I needed 3 days of dialysis." That’s not an outlier. It’s a pattern.
Who’s Most at Risk?
Some people are far more likely to develop this. Age matters. If you’re over 65, your risk is more than triple that of someone younger. Women have a 70% higher chance than men. And if you have kidney problems-even mild ones-your risk jumps 4.5 times.But the biggest risk factor? Taking five or more medications. People on polypharmacy are 17 times more likely to develop drug-induced rhabdomyolysis. That’s not just a number. It’s your grandma on statins, blood pressure pills, antibiotics, pain meds, and gout treatment-all at once. No one’s checking how they interact.
Genetics play a role too. A specific gene variant (SLCO1B1*5) makes simvastatin 4.5 times more likely to cause muscle damage. It’s common in Europeans. But most doctors don’t test for it.
How Is It Diagnosed?
There’s no single test. But doctors look for three things:- High creatine kinase (CK): Levels over 1,000 U/L are a red flag. Severe cases often hit 5,000 to 100,000 U/L.
- Dark urine: Myoglobin turns it brown or cola-colored. But don’t wait for this-it’s often absent.
- Symptoms: Pain, weakness, nausea, confusion, or decreased urine output.
CK levels rise within 12 hours of muscle damage and peak around 24 to 72 hours. They drop slowly-so one normal test doesn’t rule it out. You need repeat tests.
Other clues: high potassium (dangerous for your heart), low calcium (causes cramps), and signs of kidney failure. A urine dipstick might show blood-but no red blood cells under the microscope. That’s a telltale sign of myoglobin, not bleeding.
What Happens When You Go to the Hospital?
Time is everything. Treatment starts the moment rhabdomyolysis is suspected:- Stop the bad drug: Immediately. No delays.
- IV fluids: At least 3 liters in the first 6 hours, then 1.5 liters per hour. Goal: urine output of 200-300 mL/hour. This flushes out toxins before they wreck your kidneys.
- Urine alkalinization: Sodium bicarbonate is added to IV fluids to keep urine pH above 6.5. This stops myoglobin from clumping in the kidneys.
- Monitor electrolytes: High potassium can stop your heart. Low calcium can cause seizures. Both need urgent correction.
- Dialysis: Needed if kidneys fail. About 20-30% of severe cases require it.
The Cleveland Clinic’s protocol is clear: If CK is above 5,000 U/L, start aggressive hydration and bicarbonate right away. Don’t wait for kidney damage to appear.
Recovery-and the Long-Term Cost
If caught early, most people recover. But it’s not quick. In cases without kidney damage, full muscle strength returns in about 12 weeks. If you needed dialysis? It takes nearly 30 weeks.And it’s not just about recovery. About 44% of survivors still feel weak six months later. Some never fully regain their strength. That’s not just physical. It’s emotional. It’s financial. A single hospital stay for rhabdomyolysis costs an average of $28,743 in the U.S. And that’s just the tip of the iceberg.
Long-term, the problem is getting worse. As people live longer and take more medications, the risk climbs. Studies predict a yearly 8.2% increase in cases by 2030-unless we change how we prescribe.
How to Protect Yourself
You can’t avoid all meds. But you can avoid preventable disasters:- Ask your doctor: "Could this new drug interact with anything I’m already taking?" Don’t assume they know.
- Know your statin: Simvastatin is riskier than rosuvastatin or pravastatin. Ask if you can switch.
- Check for CYP3A4 inhibitors: These include clarithromycin, itraconazole, fluconazole, grapefruit juice, and even some antidepressants. Avoid them with statins.
- Watch for early signs: Unexplained muscle soreness, especially after starting a new drug. Don’t brush it off.
- Use a medication list: Bring it to every appointment. Even if you think it’s "just vitamins."
Pharmacists are your allies. Ask them to run a drug interaction check every time you get a new prescription. Most pharmacies have software that flags these risks. But they won’t do it unless you ask.
What’s Being Done?
Regulators are waking up. The FDA now requires statin labels to warn about CYP3A4 inhibitors. The EMA banned some dangerous combos outright. And the NIH is funding a real-time alert system to warn doctors before they prescribe risky combinations.But until that system is nationwide, the burden is on you. You’re the only one who knows what’s in your medicine cabinet. You’re the only one who can speak up.
Don’t wait for dark urine. Don’t wait for dialysis. If your muscles hurt after starting a new pill-get it checked. Fast.
Can rhabdomyolysis happen from one new medication, or only from interactions?
It can happen from a single drug, but interactions make it far more likely. Statins alone can cause rhabdomyolysis in about 1 in 10,000 users per year. But when combined with drugs like clarithromycin or gemfibrozil, the risk jumps 15 to 20 times higher. Most cases are triggered by drug combinations, not single agents.
I take statins and have muscle pain. Should I stop them?
Don’t stop without talking to your doctor. Muscle pain is common with statins, but rhabdomyolysis is rare. If your pain is new, severe, or accompanied by dark urine or weakness, get a CK blood test. Your doctor might switch you to a safer statin like pravastatin or rosuvastatin, which have lower interaction risks.
Is grapefruit juice really dangerous with statins?
Yes-especially with simvastatin, atorvastatin, and lovastatin. Grapefruit juice blocks the CYP3A4 enzyme in your gut, causing up to 15 times more statin to enter your bloodstream. Even one glass a day can be risky. Switch to orange juice or avoid it entirely if you’re on these statins.
Can rhabdomyolysis cause permanent damage?
Yes. About 44% of survivors still have muscle weakness six months later. If kidney damage occurred, recovery takes longer-often over 6 months. In rare cases, permanent muscle loss or nerve damage can happen. Early treatment reduces this risk significantly.
Are there blood tests to predict who’s at risk before taking statins?
There’s a genetic test for SLCO1B1*5, which increases simvastatin risk by 4.5 times. But it’s not routine. Most doctors don’t order it because it’s expensive and not covered by insurance. If you have unexplained muscle pain on statins, ask if genetic testing might help. It’s not standard-but it’s available.
How do I know if my doctor is aware of these risks?
Ask directly: "Could my current medications interact and cause muscle breakdown?" If they can’t name the top 3 dangerous combos-statin + clarithromycin, statin + gemfibrozil, statin + itraconazole-they may not be up to date. Bring printed info from reputable sources like the FDA or Cleveland Clinic. Your life depends on it.
If you’re on multiple medications, especially if you’re over 65 or have kidney issues, don’t assume safety. Ask. Check. Speak up. Rhabdomyolysis doesn’t come with a warning label you can see. But you can learn to see the signs.
Janette Martens
December 30, 2025 AT 09:46Marie-Pierre Gonzalez
January 1, 2026 AT 02:44Louis Paré
January 2, 2026 AT 21:20Mimi Bos
January 2, 2026 AT 23:38Payton Daily
January 3, 2026 AT 18:40Kelsey Youmans
January 5, 2026 AT 00:00Teresa Marzo Lostalé
January 6, 2026 AT 10:31Gran Badshah
January 6, 2026 AT 22:27Ellen-Cathryn Nash
January 7, 2026 AT 19:38Sydney Lee
January 8, 2026 AT 14:38oluwarotimi w alaka
January 9, 2026 AT 12:02Debra Cagwin
January 10, 2026 AT 17:03